Bio-Med 281
Cardiac Pathophysiology Exam
September 24, 2001
Course Directors:
Douglas Burtt, M.D.
Lauralyn Cannistra, M.D.
Questions 1 – 4: A fifty-five year old male presents to the Emergency Room with recent onset of dyspnea on exertion, orthopnea and PND (paroxysmal nocturnal dyspnea). On examination he has the following findings:
Vitals: Pulse 140 irregularly irregular; BP: 130/100; Resp rate: 24/min.; afebrile
Neck: 6 cm JVD, with delay of the carotid upstrokes
Chest: Rales ¼ of the way up, bilaterally
Cor: Irregular S1 and S2; III/VI late-peaking systolic ejection murmur at the base, radiating to the carotids
1. On the two ventricular compliance curves shown below, at which location was this patient most likely to be at the time of initial presentation:
a) Point A
b) Point B
c) Point C
d) Point D

2. Treating this patient with a diuretic would cause the following change:
a) the patient would move from the upper curve to the lower curve, at the same vertical position
b) the patient would move from the lower curve to the upper curve, at the same vertical position
c) the patient would stay on the same curve and move up and to the right
d) the patient would stay on the same curve and move down and to the left
3. On echocardiography, this patient is most likely to have which of these findings:
a) elongated and thinned chordae tendinae with rupture of several of the chordae
b) thickening of the upper portion of the intraventricular septum with obstruction of ventricular outflow beneath the aortic valve
c) thickened mitral valve leaflets and sub-mitral apparatus with “doming” of the mitral valve leaflets
d) a bicuspid aortic valve with thickened leaflets and decreased opening of the leaflets
e) billowing and redundant mitral leaflets with mitral prolapse
4. This patient’s heart rhythm may cause all of the following, except:
a) predisposition to thrombo-embolism originating in the left atrium
b) reduced cardiac output due to loss of the “atrial kick”
c) reduced stroke volume due to increased heart rate
d) predisposition to development of sudden death with ventricular fibrillation
e) variation in intensity of the murmur from beat to beat
![]()
Questions 5 – 6:
A 42-year-old male smoker with a history of hypercholesterolemia presents to the hospital with recent onset of mid-sternal chest pressure occurring with minor physical activity, and, on several occasions, awakening him from sleep.
5. All of the
following statements about this patient’s intracoronary adenosine levels and
the effect of adenosine on the coronary are true, except:
a) adenosine binds to receptors on the endothelium and increases calcium entry into the cell
b) adenosine is a prime mediator of coronary vascular tone
c) adenosine is a potent coronary vasodilator
d) adenosine’s effect on coronary vascular tone is opposite to the effect of oxygen
e) more adenosine is produced when aerobic metabolism is inhibited
6. All of the following statements about the coronary obstruction causing this patient’s symptoms are true, except:
a) there was likely to have been a soft, lipid-laden atherosclerotic plaque recently present at the site of the current obstruction
b) there is likely to be an occlusive thrombus at the site of obstruction
c) there is likely to be a component of coronary vasospasm at or near the site of obstruction, due to dysfunctional endothelium
d) there is likely to be increased platelet aggregation at a site of plaque disruption
e) treatment of the patient with aspirin will render the site of obstruction less likely to occlude completely
![]()
Questions 7 – 12: The following diagram depicts jugular venous pressure tracings in a normal individual (diagram A), and in two patients with pericardial disease (B and C). Please answer the True/False questions below, based on this diagram:
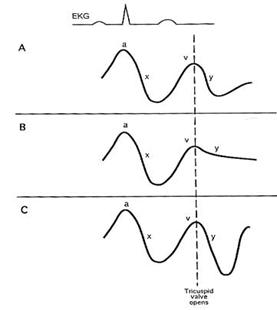
Answer True or False (A = True, B = False):
7. The patient depicted in panel B may have pericardial tamponade, based on the blunted y-descent shown
8. The patient in panel B is likely to exhibit elevated overall jugular venous pressure.
9. The patient in panel B is likely to exhibit pulsus paradoxus.
10. The patient in panel C may have pericardial constriction, based on the rapid y-descent.
11. The patient in panel C is likely to exhibit elevated overall jugular venous pressure.
12. The patient in panel C is likely to exhibit pulsus paradoxus.
![]()
Question 13 – 17: A patient with hypertrophic cardiomyopathy with outflow tract obstruction may have a crescendo-decrescendo systolic murmur, which may vary with various maneuvers. Please answer the following questions True or False (A = True; B = False):
13. Administration of an inotropic drug (e.g. Epinephrine) increases the murmur.
14. The Valsalva maneuver increases the murmur.
15. Squatting increases the murmur.
16. Administration of a veno-dilator (e.g. nitroglycerine) increases the murmur.
17. Administration of an arterial vasodilator (e.g. hydralazine) increases the murmur.
18. Gradual acceleration at the onset of a tachycardia is most characteristic of which tachycardia mechanism:
a. Automaticity
b. Reflection
c. Triggered activity
d. Reentry
19. Which of the following statements about reentrant arrhythmias is true?
a. A fully excitable gap is always present.
b. Unidirectional block must be present permanently in part of the circuit.
c. Initiation requires a critical degree of conduction slowing in part of the circuit.
d. The location of the site of unidirectional block required for initiation of reentry is usually the same as the site of critical conduction slowing.
20. An example of a common reentrant arrhythmia utilizing a fixed anatomic barrier is:
a. Ventricular tachycardia following remote myocardial infarction
b. Atrial fibrillation
c. AV node reentry
d. Reentry utilizing a bypass tract
21. The AV node is a requisite component of the reentrant circuit in:
a. Atrial fibrillation
b. Atrial flutter
c. Orthodromic tachycardia associated with Wolff-Parkinson-White Syndrome
d. Ventricular tachycardia following remote myocardial infarction
e. Intra-atrial reentry
22. The duration of the PR interval reflects conduction through primarily:
a. Sinus node
b. Atrium
c. AV node
d. His bundle
e. Purkinje system
23. The current responsible for depolarization of atrial and ventricular myocardial cells is carried predominantly by which ion?
a. Sodium
b. Calcium
c. Magnesium
d. Potassium
e. Lithium
24. The current responsible for depolarization of sinus and AV node cells is carried predominantly by which ion?
a. Sodium
b. Calcium
c. Magnesium
d. Potassium
e. lithium
25. In critical mitral stenosis, the A2-OS (opening snap) interval is:
a. directly proportional to the length of the diastolic rumble
b. inversely proportional to the severity of stenosis
c. best heard when the valve is heavily calcified
d. all of the above
e. none of the above
26. All of the following are clinical examples of right ventricular volume overload (RVVO), except:
a. Tricuspid insufficiency.
b. Atrial septal defect with left-to-right shunting.
c. Congenital ventricular septal defect with right-to-left shunting.
d. Anomalous pulmonary venous connection to the right atrium.
27. Causes of acute mitral regurgitation include all of the following, except:
a. Bacterial endocarditis
b. Ruptured chordae tendineae
c. Acute MI with papillary muscle rupture
d. Ischemic papillary muscle dysfunction
e. Rheumatic mitral valve disease
![]()
Questions 28 – 31: Match the beneficial effect on heart failure with the drug treatment:

28. point a ® point b
29. point a ® point c
30. point a ® point d
31. point a ® point e
a. Digoxin
b. Vasodilators
c. Diuretics
d. Digoxin and vasodilators
![]()
32. A 17 year-old male has fatigue. Clinical examination reveals jugular venous distension, mild peripheral edema, and hepatomegaly. Right heart catheterization reveals:
RA pressure = 23 mm Hg
RV pressure = 60/23 mm Hg
PCW pressure = 20 mm Hg
Cardiac index = 1.7 L/min/m2
The hemodynamic data are consistent with:
- Restrictive Cardiomyopathy
- Constrictive Pericarditis
- Cardiac Tamponade
- All of the above
- None of the above
33. A one-year-old boy has a congenital ventricular septal defect. Which of the following is not a determinant of the amount and direction of shunted blood flow through the abnormal communication?
a. The size of the defect
b. The location of the defect
c. The pulmonary vascular resistance
d. The aortic (systemic) vascular resistance
![]()
Questions 34 – 37:

 a. b.
a. b.


c. d.
Match the disease with the hemodynamic profile:
34. Restrictive Cardiomyopathy
35. Hypertrophic cardiomyopathy
36. Tamponade
37. Constrictive Pericarditis
![]() 38. Eisenmenger’s syndrome occurs when:
38. Eisenmenger’s syndrome occurs when:
a. A congenital membranous VSD spontaneously closes around 12 months of age
b.
RV compliance exceeds
c. Atrial fibrillation occurs in Tetralogy of Fallot
d. Pulmonary hypertension from the chronic shunt overload leads to right-to-left shunting
e. A cleft mitral valve occurs in association with a VSD
39. The Fick Method of determining cardiac output predicts all of the following, except:
a. An increase in mixed venous oxygen saturation suggests an increase in cardiac output
b. A decrease in oxygen consumption suggests an increase in cardiac output
c. The cardiac output can be estimated using three parameters: the oxygen consumption, the arterial oxygen saturation and the mixed venous oxygen saturation
d. The calculation of the cardiac output using the Fick method is independent of the ability of the lungs to oxygenate the blood
![]()
Questions 40 – 42:
A normal patient has a baseline pressure-volume loop shown below (labeled "Baseline").

40. The pressure-volume loop labeled "X" might be generated by:
a. giving volume
b. giving an ACE-inhibitor
c. giving a diuretic
d. giving an inotropic agent
41. The pressure-volume loop labeled "Y" might be generated by:
a. giving volume
b. giving an ACE-inhibitor
c. giving a diuretic
d. giving an inotropic agent
42. The distance "Z" (shown by
the labeled double arrow) represents:
a. cardiac output
b. preload
c. afterload
d. stroke volume
e. end-systolic volume
![]()
Questions 43 – 47:
A 78 year-old female with long-standing hypertension presents to the hospital with the acute onset of mid-sternal chest pressure and dyspnea. Pertinent physical findings include:
Heart rate: 110, regular; Blood Pressure: 200/90; Respirations: 24
Neck: 10 cm of JVD; normal upstrokes
Chest: Rales ½ of the way up bilaterally
Heart: Rapid S1 and S2 with a II/VI holosystolic murmur at the apex, radiating towards the axilla
Extremities: no edema, cyanosis or clubbing
The electrocardiogram reveals sinus tachycardia with ST elevation consistent with an acute anterior myocardial infarction.
43. The imaging study that would be most appropriate for evaluation of her systolic murmur would be:
a. Thallium stress test
b. Resting technetium scan
c. Transthoracic echocardiography
d. Right heart catheterization
e. Coronary angiography
44. All of the following statements about her acute myocardial infarction are true, except:
a. the “ischemic cascade” starting at the onset of her myocardial infarction includes diastolic dysfunction, systolic dysfunction, EKG changes and chest pain
b. the myocardial infarction proceeds in a “wavefront” manner, proceeding from epicardium to endocardium
c. systolic dysfunction caused by the infarction may lead to further ischemia by decreasing coronary perfusion pressure
d. diastolic dysfunction caused by the infarction may lead to increased wall tension and decreased oxygen delivery to the myocardium
e. sympathetic stimulation due to the pain of the infarction may increase myocardial oxygen demand (MVO2)
Several days after hospitalization, the patient becomes more dyspneic and her systolic murmur is now noted to be louder and harsher. A right heart catheterization reveals the data shown below:
|
|
Oxygen Saturation |
Pressure (mm Hg) |
|
Right Atrium |
59% |
8 |
|
Right Ventricle |
72% |
40/8 |
|
Pulmonary Artery |
74% |
40/22 |
|
Pulmonary Capillary Wedge |
|
25 mean V-waves to 30 |
45. This patient's echocardiogram might be expected to show:
- Acute ventricular septal defect
- Acute mitral regurgitation
- Acute left ventricular free wall rupture
- Acute right ventricular infarction
- Acute left ventricular apical aneurysm formation
46. The likely gross pathologic finding in the affected portion of this patient's heart muscle is:
- White, fibrotic thinned myocardium
- Red, hemorrhagic thickened myocardium
- Normal appearing myocardium
- Purple, discolored firm myocardium
- Yellow, softened myocardium
47. Treatment of the patient at this time might include all of the following, except:
a. adminstration of thrombolytic therapy
b. emergency cardiac catheterization
c. placement of an intra-aortic balloon pump
d. surgical consultation for possible open-heart surgery
e. vasodilatory drugs to augment forward cardiac output
![]()
Questions 48 – 50:
A 48-year-old Saudi Arabian female with a history of rheumatic fever at age 20 presents to the office with progressive fatigue and dyspnea on exertion. Physical examination reveals:
Heart rate: 90, regular; Blood Pressure: 120/70; Respirations: 18
Neck: 8 cm JVD with prominent jugular V-waves; normal carotid upstrokes
Chest: Fine rales at the bases
Cor: Prominent S1, increased pulmonic component of S2; high-pitched snap shortly after S2; soft, II/VI systolic blowing murmur at the left sternal border, increasing with inspiration; soft diastolic rumble with pre-systolic accentuation
Extremities: trace edema; no cyanosis
48. One would expect that this patient’s valvular abnormalities would include:
a. Mitral stenosis and tricuspid insufficiency
b. Aortic insufficiency and mitral regurgitation
c. Aortic stenosis and mitral regurgitation
d. Mitral stenosis and aortic insufficiency
e. Hypertrophic cardiomyopathy with outflow tract obstruction
49. On echocardiography, one would expect that this patient’s left ventricle would demonstrate:
a. Concentric left ventricular hypertrophy
b. Cavity dilation and global left ventricular hypokinesis
c. Normal cavity size and normal left ventricular function
d. Discrete sub-aortic septal hypertrophy
e.
50. Cardiac catheterization might demonstrate a gradient between which two pressures:
a. Left ventricular and pulmonary capillary wedge pressure during diastole
b. Ascending aortic pressure and left ventricular pressure during systole
c. Right atrial and right ventricular pressure during diastole
d. Right ventricular and pulmonary artery pressure during systole
e. Left ventricular and left atrial pressure during systole
![]()

(This diagram of
normal pressures is included for your reference)