Bio-Med
Combined
Cardiac Pathophysiology,
Pharmacology &
Pathology Exam
September
24th, 2002
Course
Directors:
Pharmacology
|
Pathophysiology
|
Pathology
|
Robert Patrick, Ph.D.
|
Douglas Burtt, M.D.
|
Kim Boekelheide, M.D., Ph.D.
|
|
|
|
|
|
|
Hank Wu, M.D.
|
|
Wisdom begins in
wonder
Socrates
Questions 1 – 5:
A 58 year old male with a history of a heart murmur since adolescence is referred to your office for worsening dyspnea on exertion. Physical examination reveals:
Heart rate: 96 and regular Blood Pressure: 180/60 Resp rate: 20
Neck: No jugular venous distension; bounding carotid upstrokes
Chest: clear to auscultation
Cardiac:
a II/VI early peaking systolic ejection murmur at the base, radiating to the neck;
a III/VI diastolic decrescendo blow at the left sternal border;
positive S4 gallop, but no S3 gallop.
Extremities: No edema, cyanosis or clubbing.
Chest X-ray reveals an enlarged cardiac silhouette, with normal lung fields.
1.
All of the following statements about this patient’s echocardiographic
findings are likely to be true, except:
a) left ventricular dimensions are likely to be enlarged
b) left ventricular diastolic compliance is likely to be impaired
c) the mitral valve apparatus is likely to be thickened and shortened
d) the aortic valve is likely to be bicuspid
e) the left ventricular systolic function may be normal
2. Treatment of this patient with all of the following agents may be beneficial, except for:
a) afterload reducing agents
b) beta-blockers
c) angiotensin converting enzyme (ACE) inhibitors
d) prophylactic antibiotics prior to dental manipulations
3. The systolic murmur heard in this patient indicates:
a) abnormally increased flow across the aortic valve
b) hypertrophic cardiomyopathy with outflow tract obstruction
c) the likelihood of a significant degree of aortic stenosis
d) pulmonic stenosis
e) tricuspid insufficiency
4. The low diastolic blood pressure noted is due to:
a) the patient’s relatively young age and lack of atherosclerosis
b) a compensatory mechanism to reduce afterload on the left ventricle
c) “forward failure” of the left ventricle
d) backflow from the aorta into the left ventricle during diastole
e) a diet low in salt and excess fluids
5. If this patient were to be treated with an angiotensin converting enzyme (ACE) inhibitor, all of the following statements would be correct EXCEPT:
a) Enalapril is an example of this type of drug
b) These drugs can cause a dry cough as a side effect
c) These drugs are safe to take during pregnancy
d) These drugs cause vasodilation
e) These drugs inhibit aldosterone production
![]()
Questions 6 - 17:
A 65 year old male with longstanding poorly controlled hypertension presents to the hospital with palpitations and shortness of breath. On examination he has signs of mild congestive heart failure, with rales at the lung bases and is noted to have an irregularly irregular pulse. His blood pressure is elevated at 190/95 mm Hg.
A bedside echocardiogram reveals concentric left ventricular hypertrophy without significant valvular abnormalities. An EKG reveals an irregularly irregular rhythm without discernible P waves, with a rate of 130/minute.
6. This patient's heart rhythm most likely is:
a) multifocal atrial tachycardia
b) ventricular tachycardia
c) atrial fibrillation
d) sinus arrhythmia
e) sinus tachycardia
7. This patient is likely to have all of the following hemodynamic features, except:
a) decreased filling of the left ventricle due to increased heart rate
b) markedly decreased left ventricular ejection fraction
c) loss of the atrial “kick”, causing loss of the “a” wave
d) increased LVEDP, due to decreased compliance
e) increased
8. Compared to a patient with aortic stenosis, this patient would have all the same features except:
a) minimal responsiveness to pharmacologic afterload reduction
b) left ventricular hypertrophy as a compensatory mechanism for increased afterload
c) predisposition for atrial arrhythmias due to left atrial enlargement
d) relatively higher left ventricular end diastolic pressure, compared to normal individuals
e) significantly reduced cardiac output would occur with loss of atrial "kick"
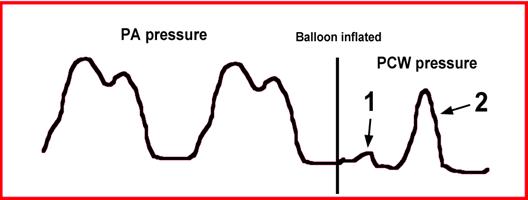
9. At which point on the two ventricular compliance curves shown above was this patient most likely to be at the time of initial presentation:
a) Point A
b) Point B
c) Point C
d) Point D
10. Treating this patient with an infusion of fluid would cause the following change:
a) the patient would move from the upper curve to the lower curve, at the same vertical position
b) the patient would move from the lower curve to the upper curve, at the same vertical position
c) the patient would stay on the same curve and move up and to the right
d) the patient would stay on the same curve and move down and to the left
e) the patient would move from the upper curve to a new curve, displaced upwards and to the left
11. Each of the following medical therapies should help this patient, except:
a) Digoxin, in order to decrease the heart
rate, and therefore improve
b) Diuretics, to reduce the
c) Arterial vasodilators, to reduce blood pressure, and, therefore, afterload
d) Sympathetic stimulants, in order to augment cardiac output
e) Nitrates, in order to reduce preload and any subendocardial ischemia
12. Pathophysiologically, the patient's left ventricular hypertrophy acts as a compensatory mechanism by:
a) reducing wall tension by lowering left ventricular pressure
b) reducing ischemia by allowing less compressive resistance to coronary blood flow
c) decreasing cardiac output by decreasing stroke volume and thereby decreasing cardiac work
d)
reducing wall tension by increasing
e) reducing myocardial oxygen demand
13. In this case, all of the following adaptive changes in cardiac myocytes would be expected except:
a) increase in length and diameter of myocardial fibers
b) additional sarcomeres
c) decreased contractile-related mRNA and proteins
d) increase in size of myocyte nuclei with increased DNA content
e) increase in number of mitochondria
14 – 17:
If you judge this patient to be exhibiting atrial arrhythmia,
you could treat with anti-arrhythmic medication. For the numbered
anti-arrhythmic drugs below, match up the single most appropriate lettered
description. Each lettered description may be used once, more than once, or not
at all.
14. Lidocaine
15. Atenolol
16. Amiodarone
17. Verapamil
a) an agent with class III activity (Vaughan Williams classification) and a half-life of greater than 14 days
b) a sodium channel blocker
c) a phosphodiesterase inhibitor
d) a calcium channel blocker
e) a b1 receptor antagonist
Questions 18 – 22:
A 36 year-old female forest ranger presents to the hospital with exertional dyspnea, fatigue and mild ankle edema. On examination, she is noted to have the following:
Pulse: 110 and regular BP: 100/70 Respiration: 20
Neck: 10 cm jugular venous distension with hepato-jugular reflux
Chest: decreased breath sounds and dullness to percussion at both bases, with rales above the area of dullness
Cardiac: Soft S1 with paradoxical splitting of S2; S3 and S4 gallops are present; no murmur or rub is present. The PMI is displaced laterally.
Abdomen: mild hepatomegaly
Extremities: 1+ ankle edema bilaterally
Electrocardiogram reveals sinus tachycardia at 110 per minute with complete left bundle branch block. Echocardiography reveals a dilated, diffusely hypocontractile left ventricle with an ejection fraction of 20%. Mild mitral regurgitation is present. No effusion is seen.
18. In patients such as this one, one may find any of the following except:
a) Pulsus alternans
b) Pulsus paradoxus
c) Cardiomegaly
d) Increased left ventricular end diastolic volume
e) Decreased stroke volume
19. This patient’s condition might have been caused by any of the following, except:
a) Lyme disease
b) Recent viral myocarditis
c) Heavy alcohol consumption
d) Chagas disease
e) Vitamin B-12 deficiency
20. Which of the
following would occur if this patient were to be given a cardiac glycoside such
as digoxin:
a) Decreased cardiac force of contraction (negative inotropic effect)
b) A decrease in digoxin cardiac effects if potassium depleting diuretics are used concurrently with the digoxin
c) Lowering of calcium content in the cardiac sarcoplasmic reticulum (SR)
d) Inhibition of cardiac Na+-K+ ATPase activity
e) Decrease in cardiac intracellular sodium concentration
This patient’s Frank-Starling relationship is shown below:
I IV II 30
(mm Hg) 2.5 1.5 1.0 2.0 20 10 III

![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
21. At the time of presentation above, this patient’s hemodynamics fell into which quadrant:
a) Quadrant I
b)
Quadrant II
c)
Quadrant III
d) Quadrant IV
22. The use of what pharmacologic or therapeutic intervention might bring the patient from point B to point A on the curve:
a) Digitalis
b) Epinephrine
c) Volume infusion
d) A diuretic
e) A beta-blocker
Questions 23 – 27:
Match each question with the single best answer (A - E).
|
23. Impaired diastolic filling of ventricles; jugular venous pressure with rapid “y descent”; left ventricular pressure tracing with “dip and plateau” configuration |
A) Cardiac
tamponade |
|
24. Impaired diastolic filling of left ventricle; systolic anterior motion of the mitral valve; systolic murmur which accentuates with standing up |
B)
Restrictive cardiomyopathy |
|
25. Impaired diastolic filling of ventricles; cyclical decrease in systolic blood pressure during inspiration; elevated jugular venous pressure without Kussmaul’s sign |
C)
Hypertrophic cardiomyopathy |
|
26. Impaired diastolic filling of the left ventricle; loud first heart sound (S1); increased pulmonary venous pressure with occasional “reactive” pulmonary hypertension |
D)
Constrictive pericarditis |
|
27. Impaired diastolic filling of the ventricles; fibrosis, scarring, or infiltration of the myocardium; normal pericardial tissue |
E) Mitral
stenosis |
28. A 42 year-old female presents to the hospital with signs and symptoms of right heart failure (distended neck veins, pleural effusions, ankle edema). An echocardiogram reveals normal left ventricular systolic function (no other data from the echo is available to you). The patient could have any of the following conditions, except:
a) Mitral stenosis
b) Ischemic cardiomyopathy
c) Cardiac tamponade
d) Constrictive pericarditis
e) Restrictive cardiomyopathy
PATH QUESTIONS 29 - 31: You are working in a Guatemalan clinic during Christmas vacation and see a 34 year old man who is febrile and appears chronically ill. He complains of joint pain. On exam, he shows chorea as well as multiple subcutaneous nodules on his arms and legs. On auscultation, he has a 2/6 diastolic murmur consistent with mitral stenosis. EKG shows a prolonged PR interval.
29. His mitral valve is replaced to relieve the stenosis. Histopathologic examination of his excised mitral valve and surrounding tissue might show all the following except:
a) Aschoff bodies
b) Neovascularization
c) Fibrosis
d) T cell infiltrates
e) Streptococci
30. When examined, his excised mitral valve shows characteristic vegetations. These are most likely to be:
a) Small, warty vegetations along the line of closure
b) Large, irregular masses on the valve cusps
c) Medium-sized vegetations on both sides of the valve leaflet
d) Erosive masses of bacteria
e) Bland accumulations of fibrin which are non-destructive
31. The most likely diagnosis is:
a) Acute rheumatic heart disease
b) Chronic rheumatic heart disease
c) Acute and chronic rheumatic heart disease
d) Infective endocarditis
e) Luetic pancarditis
Questions 32 – 39 (questions 37 – 39 are related to figure 1):
A 60 year-old male smoker presents to the hospital with the abrupt onset of severe substernal chest pressure with radiation to the left arm, associated with diaphoresis and dyspnea and cool extremities. An electrocardiogram reveals sinus tachycardia (heart rate = 110/minute) with ST-segment changes consistent with an acute anterior myocardial infarction.
32. All of the following statements about this patient’s MI are true, except:
a) the rapid heart rate may be a compensatory mechanism for decreased stroke volume
b) the rapid heart rate may suggest impending complete heart block
c) the dyspnea may reflect increased left ventricular end diastolic pressure
d) the chest discomfort may be due to occlusion of the left anterior descending coronary artery
e) the cool extremities are likely due to increased catecholamines causing vasoconstriction
33. The pathophysiologic mechanisms of this MI may include all of the following, except:
a) local inflammation in the wall of the coronary artery involving active macrophages
b) a non-occlusive thrombus partially obstructing blood flow to the myocardium
c) recently fissured or ruptured eccentric coronary atheromatous plaque
d) local vasoconstriction due to decreased local levels of EDRF
e) the presence of foam cells displaying tissue factor, a potent clot promoter
34. Potential mechanical complications occurring several days following the myocardial infarction include all of the following, except:
a) acute right ventricular infarction, causing hypotension and JVD
b) acute ventricular septal defect, causing dyspnea and a new murmur
c)
acute
d) acute mitral regurgitation, with a flail mitral leaflet
e) left ventricular apical aneurysm formation, with possible thrombus formation
35. In which coronary artery or branch are we likely to find a thrombus with this infarct?
a) A-V nodal branch
b) Left anterior descending coronary artery
c) First septal perforator branch
d) Left circumflex coronary artery
e) None of the above
36. Which of the following is not a determinant of this patient's myocardial oxygen demand (MVO2)?
a) heart rate
b) contractility
c) preload
d) hemoglobin content
e) afterload
The patient expired. Shown in Figure 1 is a photomicrograph of a portion of the patient’s heart obtained at autopsy. The inset is a higher magnification of an area similar to that within the rectangle of the lower magnification image. Answer the following questions:
37. The cells identified with arrows in the inset are most likely:
a) Aschoff cells
b) polymorphonuclear leukocytes
c) macrophages
d) necrotic cardiomyocytes
e) endothelial cells
38. The lower portion of Figure 1, identified with the bracketed bar, is most consistent with:
a) necrotic debris
b) granulation tissue
c) acute rheumatic endocarditis
d) scar
e) hemorrhage
39. Based on this image (figure 1), approximately how long after the onset of disease did the patient die?
a) 1 hour
b) l day
c) 1 week
d) 1 month
e) 1 year
![]()
Questions 40 + 41:
40. An echocardiogram of a 25 year-old male reveals hypertrophic cardiomyopathy with obstruction. All of the following statements about the pathophysiology of this patient’s condition are true, except:
a) decreased
b) increased outflow obstruction may lead
to increased
c) increased MVO2 may lead to increased myocardial ischemia
d) small vessel disease associated with hypertrophic cardiomyopathy may cause decreased myocardial blood flow
e) impaired
41. Which gene is least likely to show evidence of mutation in this patient?
a) beta cardiac myosin
b) troponin T
c) beta amyloid
d) alpha cardiac myosin
e) alpha tropomyosin
![]()
42. Restrictive cardiomyopathy is characterized by all of the following, except:
a) biventricular heart failure, with left heart failure predominance
b) etiologies including amyloidosis and sarcoidosis
c) similar hemodynamic profile to constrictive pericarditis, with rapid “y descent” in the right atrium and “dip and plateau” rapid ventricular filling in the right ventricle
d) usually normal pericardium
e) reduced ventricular cavity sizes
43. Pericardial tamponade is associated with all of the following, except;
a) jugular venous distension
b) hypotension
c) pulsus paradoxus
d) decreased
e) inspiratory increase in jugular venous pressure
![]()
Questions 44 + 45:
44 + 45:
A 38 year old woman
presents with a blue left fifth toe. She was in good health prior to this aside
from occasional fainting spells. She had visited her gynecologist yearly.
Coagulation studies were within normal limits. An EKG was within normal limits.
An echocardiogram was performed which showed a mobile, 2.5 cm mass in the left
atrium.
44. The most likely diagnosis is:
a) Myxoma
b) Rhabdomyoma
c) Angiosarcoma
d) Metastatic carcinoma
e) Intra-atrial thrombus
45. The patient underwent complete surgical excision of the mass and tolerated the procedure well. The most likely clinical outcome is:
a) Death due to metastatic disease
b) Recurrence of the atrial mass
c) Recurrent emboli
d) No sequelae
e) Mitral valve dysfunction
![]()
46. Which phase of the action potential in pacemaker cells leads to their "automatic" depolarization?
a) Phase 0
b) Phase 1
c) Phase 2
d) Phase 3
e) Phase 4
47. All of the following are necessary for reentrant tachyarrhythmias, except:
a) Unidirectional block
b) Slowed conduction in one portion of the reentrant loop
c) AV nodal suppression
d) Pathways with differing conduction properties
e) An initiating event, usually a premature beat
48. The AV node is a requisite component of the reentrant circuit in:
a. Atrial fibrillation
b. Atrial flutter
c. Orthodromic tachycardia associated with Wolff-Parkinson-White Syndrome
d. Ventricular tachycardia following remote myocardial infarction
e. Intra-atrial reentry
49. The current primarily responsible for depolarization of atrial and ventricular myocardial cells is carried predominantly by which ion?
a. Sodium
b. Calcium
c. Magnesium
d. Potassium
50. The current responsible for depolarization of sinus and AV node cells is carried predominantly by which ion?
a. Sodium
b. Calcium
c. Magnesium
d. Potassium
![]()
51 – 53:
PATH QUESTIONS 51 - 53: A 47 year old woman presented
to the emergency room with severe “tearing” chest pain for 4 hours. She denied
previous heart disease but had not seen a physician in 5 years. On exam, her
blood pressure is 210/150 with a pulse of 92 and respirations of 30. She
appears in acute discomfort. Cardiac auscultation and EKG are within normal
limits except for evidence of left ventricular hypertrophy. She is treated with
analgesics and placed in observation; 2 hours later she is found dead. An
autopsy showed 300 cc of clotted blood in the pericardium. Answer the following
questions:
51. What is the most likely cause of death?
a) cardiac tamponade due to a ruptured myocardial infarction
b) cardiac tamponade due to a dissecting aneurysm
c) cardiac tamponade secondary to chest trauma
d) cardiac tamponade due to a ruptured atherosclerotic aneurysm
e) hemorrhagic constrictive pericarditis
52. Based on the history, what part of the cardiovascular system was most likely
the immediate source of the blood filling the pericardium?
a) the heart
b) the pulmonary artery
c) the ascending aorta
d) the aortic arch
e) the descending aorta
53. If you had been this patient’s physician, what would you have done?
a) The “wait and see” management approach to this patient was appropriate.
b) Immediate surgery should have been performed.
c) An immediate radiographic study, such as an helical CT scan of the chest, was indicated
d) An echocardiogram should have been performed to evaluate the extent of left ventricular hypertrophy
e) The pulmonary capillary wedge pressure should have been assessed to determine the extent of congestive heart failure
![]()
Questions 54 - 59 have True or False answers (1/2 point each):
Answer A for True or B for False.
There are three shunt pathways that are instrumental in the fetal circulation.
54. One of these pathways is called truncus arteriosus
55. One of these pathways is called ductus venosus
56. One of these pathways is called the interventricular foramen
57. One of these pathways is called the foramen ovale
58. One of these pathways is called septum primum
59. One of these pathways is called ductus arteriosus
![]()
60. Tetralogy of Fallot is a constellation of four associated anomalies:
a) Ventricular septal defect; pulmonic insufficiency; transposition of the great vessels; right ventricular hypertrophy
b) Atrial septal defect; tricuspid stenosis; right ventricular hypertrophy; Eisenmenger’s syndrome
c) Ventricular septal defect; infundibular, valvular or supravalvular pulmonic stenosis; an anteriorly displaced aorta that receives blood flow from both ventricles; right ventricular hypertrophy
d) Atrial septal defect; pulmonic stenosis; right ventricular hypertrophy; an anteriorly displaced aorta that receives blood flow from both ventricles
e) Ventricular septal defect; pulmonary atresia; left ventricular hypertrophy; left atrial enlargement
61. Eisenmenger’s syndrome occurs when:
a) A congenital membranous VSD spontaneously closes circa 12 months of age
b) RV compliance exceeds
c) Atrial fibrillation occurs in Tetralogy of Fallot
d) Pulmonary hypertension from the chronic shunt overload leads to right-to-left shunting
e) A cleft mitral valve occurs in association with a VSD
Questions
62 - 70:
A 50-year-old male presents to the hospital
with a large inferior myocardial infarction.
62. On initial presentation to the hospital the patient's blood pressure is low, with a reading of 90/60 mm Hg. Pathophysiologic reasons for his low blood pressure might include all of the following, except:
a) right ventricular infarction causing increased vascular resistance
b) right ventricular infarction causing
low
c) hypovolemia (low intravascular volume)
d) reduced vascular resistance from increased vagal tone
e) reduced cardiac output related to the MI
63. Therapy to treat the hypotension might include all the following, except:
a) an intra-aortic balloon pump
b) intravenous inotropic agents
c) infusion of fluids (i.e. saline solution)
d) intravenous nitroglycerine infusion
e) elevating the patient’s legs
64. The pathophysiology of his acute myocardial infarction might involve all of the following, except:
a) a "wave front" spread of ischemia and infarction from the endocardium to the epicardium
b) plaque rupture with platelet aggregation and thrombosis
c) release of serum catecholamines exacerbating ischemia
d) increase in left ventricular wall tension
e) increase in left ventricular compliance
65. True statements about the release of cardiac enzymes following this patient’s myocardial infarction include all of the following, except:
a) CPK (creatinine phosphokinase) levels usually peak 16 – 36 hours after the onset of cell injury
b) troponin I elevation is the most specific marker for cardiac cell death
c) total CPK elevation is highly specific for cardiac cell death
d) peak CPK elevation occurs earlier after successful myocardial reperfusion
e) initial CPK and troponin levels are often normal in the first hour following MI
66. All of the following are determinants of this patient's myocardial oxygen supply, except:
a) viscous coronary resistance
b) compressive coronary resistance
c) hemoglobin content
d) wall tension
e) cardiac output
On day four of the hospitalization, the patient develops a
new systolic heart murmur and the following oxygen saturations and pressure
readings are obtained with a Swan-Ganz right heart catheter:
|
|
Oxygen Saturation |
Pressure (mm Hg) |
|
Right Atrium |
62% |
8 |
|
Right Ventricle |
61% |
30/8 |
|
Pulmonary Artery |
61% |
30/22 |
|
Pulmonary Capillary Wedge |
|
22 mean V-waves to 50 |
67. This patient's echocardiogram might be expected to show:
a) Acute ventricular septal defect
b) Acute mitral regurgitation
c) Acute left ventricular free wall rupture
d) Acute right ventricular infarction
e) Acute left ventricular apical aneurysm formation
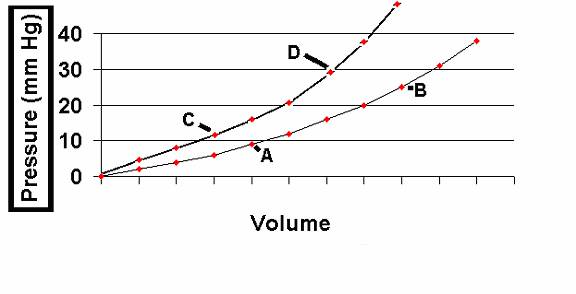
This
patient's right heart pressure tracing is seen below.
68. What is the correct title for the section labeled 1?
a) C-wave
b) The dicrotic notch
c) A-wave
d) A small V-wave
e) A “giant” V-wave
69. What is the correct title for the section labeled 2?
a) C-wave
b) The dicrotic notch
c) A-wave
d) A normal V-wave
e) A “giant” V-wave
70. All of the following imaging studies might be helpful in evaluating this patient for the reasons given, except:
a) radionuclide ventriculography (gated red-blood cell scan) to evaluate left ventricular ejection fraction and wall motion
b) coronary angiography to assess left ventricular wall motion
c) echocardiography and Doppler study to assess left ventricular systolic and diastolic function and to assess valvular function and for presence of intracardiac shunts
d) thallium stress testing to assess for residual areas of myocardial ischemia
e) left ventriculography to assess LVEDP, left ventricular systolic function and for presence of acute VSD or acute mitral regurgitation
QUESTIONS 71 - 73 ARE RELATED TO FIGURE 2:
71 - 73
A 70 year old man comes to your office with complaints of jaw and muscle pain and increasing, persistent headache. On questioning, he indicates that he has had intermittent problems reading the newspaper for the last week. He denies fever or chest pain, and had a normal physical exam approximately 1 year ago. He has taken digoxin for many years but denies taking other prescription or over the counter medications. A diagnostic biopsy is performed (Figure 2).
71. Given this history, what is the most likely source of the biopsy material?
(circle the correct answer)
a) Skin
b) Muscle
c) Temporal artery
d) Lung
e) Kidney
72. Which therapeutic option is most appropriate based on the patient’s presentation.
(circle the best answer):
a) Tylenol
b) Corticosteroid therapy
c) Discontinue digoxin
d) Erythromycin
f) Nifedipine
73. Briefly describe the histopathological features of this biopsy. Specifically comment on what is being identified with the asterisk and the arrow. Also, make sure you discuss the type of inflammatory response seen in the circled area.
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
QUESTIONS 74 - 76 ARE RELATED TO FIGURE
3:
74 - 76
The developmental origin of the normal components of the
atrial septum in the area of the foramen ovale is shown in Figure 3 (RA = right
atrium; LA = left atrium). Defects in this area are called secundum type atrial
septal defects, and are some of the most common congenital heart defects.
Answer the following questions:
74. Patent foramen ovale usually results from abnormal or excessive resorption of the septum primum during formation of the foramen secundum. Which labeled structure in “C” is affected in this disease process (CIRCLE “BLUE” OR “YELLOW”)?
BLUE
YELLOW
75. An abnormally large foramen ovale can also result from defective development of the septum secundum. Which labeled structure in “C” is affected in this disease process (CIRCLE “BLUE” OR “YELLOW”)?
BLUE
YELLOW
76. Closure of the foramen ovale (the transition from panel C to panel D) normally occurs perinatally. Briefly explain what perinatal events are associated with this transition (2-3 sentences).
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
________________________________________________________________________________________________________________________________________________
Remember that there is nothing stable in human
affairs; therefore avoid undue elation in prosperity, or undue depression in
adversity.
Socrates