Langerhans
Cell Histiocytosis
The
patient was a 55 year old male smoker with history of an undifferentiated
carcinoma of small bowel with involvement of the adjacent pancreas and grossly
positive surgical margin at the time of resection.
Follow up was unremarkable until six years later
when he developed multiple small nodules in the right lower lobe of the lung
which appeared to be growing in size with central cavitation. The radiological
differential diagnosis included metastatic carcinoma, primary lung adenocarcinoma
and benign lesions (eosinophilic granuloma, etc.). A wedge resection was
performed.

Resection revealed multiple
white well circumscribed nodules ranging from 0.4 to 0.8cm occupying
approximately 80% of the lung wedge. The remaining lung parenchyma appeared
grossly congested.
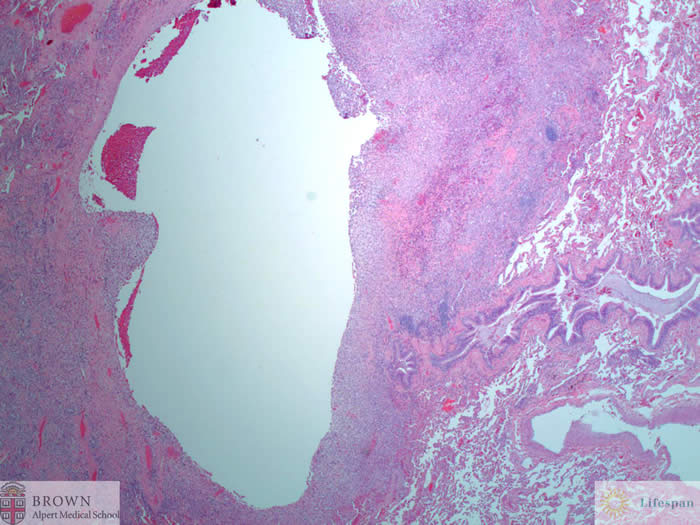
Microscopically, the
lesions were comprised of nodular aggregates of large foamy histiocytic cells
with associated pigment laden macrophages, lymphocytes and eosinophils
surrounding a central cavity.
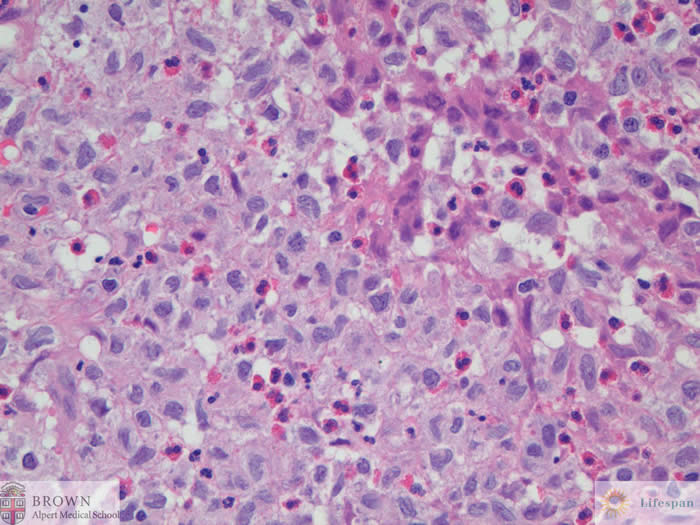
The larger cells had
pale eosinophilic cytoplasm with sharp nuclear infoldings and conspicuous
mitotic activity (not shown).
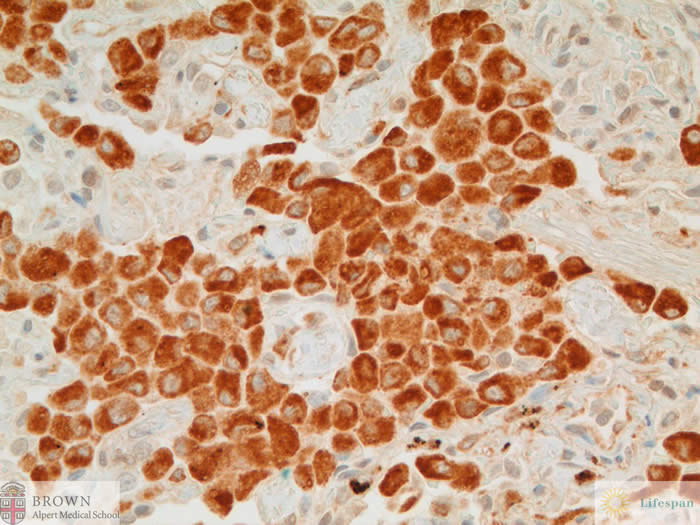
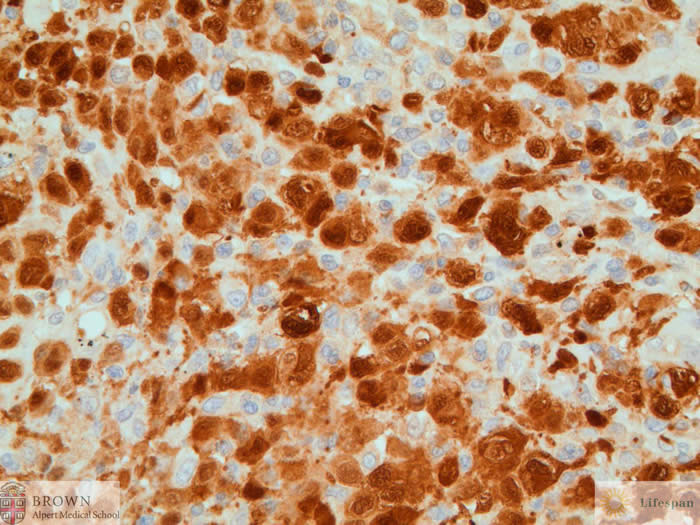
CD68 highlights the
lesional cells.
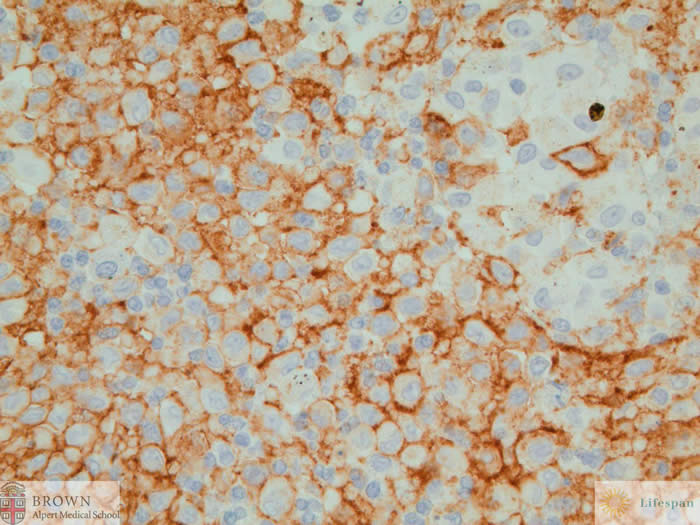
CD1a highlights the
lesional cells.
S100 highlights the
lesional cells.
The lesional cells were positive for S100, CD1a
and CD68. They were negative for keratin cocktail, TTF1, P63, CK5/6, Calretinin
and EMA. The proliferation index was increased, at approximately 15%. The
morphology and immunohistochemical phenotype was supportive of a diagnosis of
Langerhans cell histiocytosis. Surgical margin was free from the lesion.
Adequate sampling did not reveal any residual carcinoma.
The diagnosis is Langerhans cell histiocytosis.
Pulmonary Langerhans cell histiocytosis
predominantly affects young adults between the ages of 20 - 40 years. The
pathologic hallmark is the accumulation of Langerhans and other inflammatory
cells in the small airways, resulting in a nodular distribution of disease.
Eventual destruction of bronchiolar walls leads to the characteristic finding
of cavitation on imaging. The majority of patients who develop this entity are
smokers but the mechanism by which this entity comes about is still unknown.
Cessation of smoking has been found to lead to complete or partial remission of
the disease. Langerhans cells, being histiocytes, are positive for histiocyte
marker CD68 but are also characteristically positive for both CD1a and S100.
Contributed by Sonja
Chen, MD and Dr. Ali Amin