Castleman's Disease
An 87-year-old male with history of myelodysplasia (Refractory cytopenia with multilineage dysplasia with inv(3)(q21q26.2)) was presented with right axilla lymphadenopathy. No typical B symptom was noted. An excisional biopsy of the lymph node was performed.
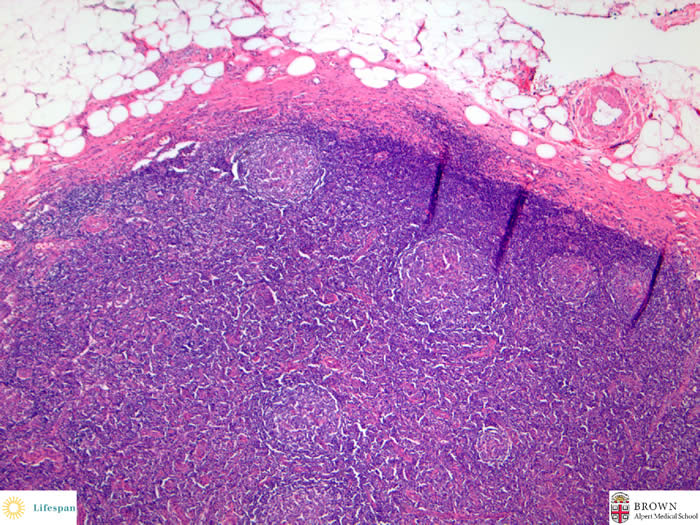
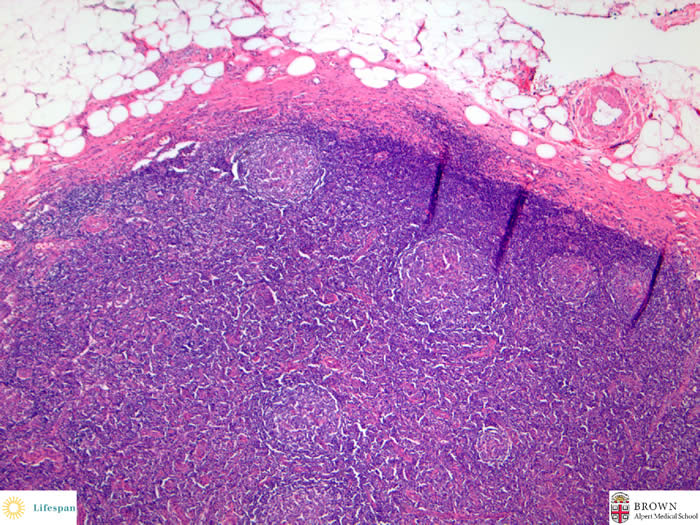
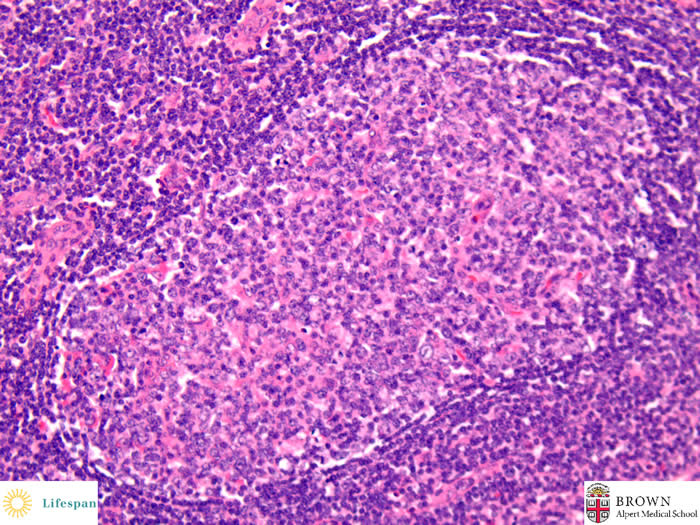
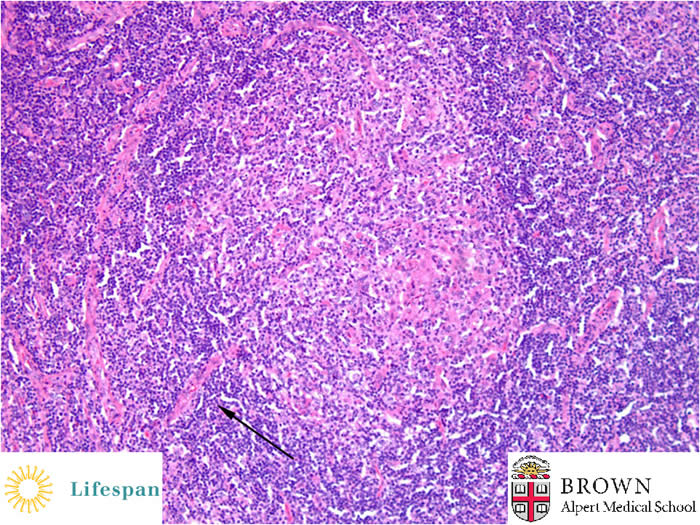
The capsule of the lymph node is thickened. The sinuses are obliterated.
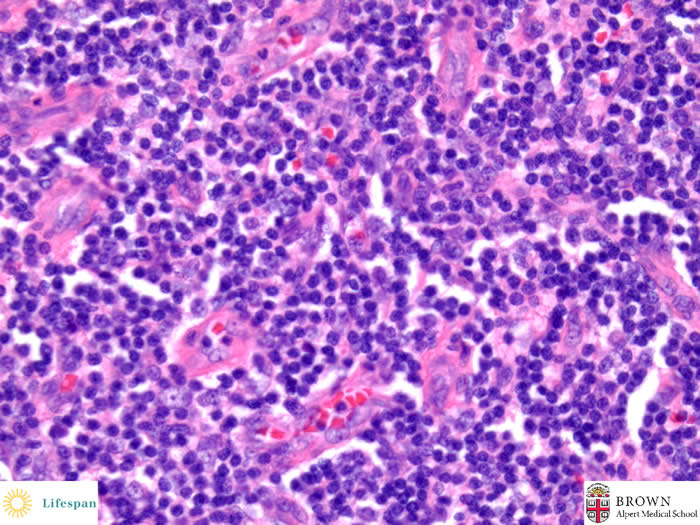
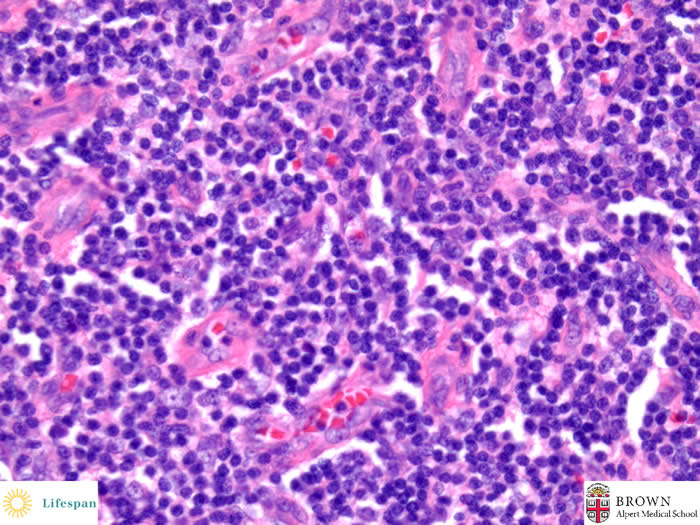
There is a pronounced proliferation of blood vessles with hylinized walls and lined by plump endothelial cells in the inter-follicular area.
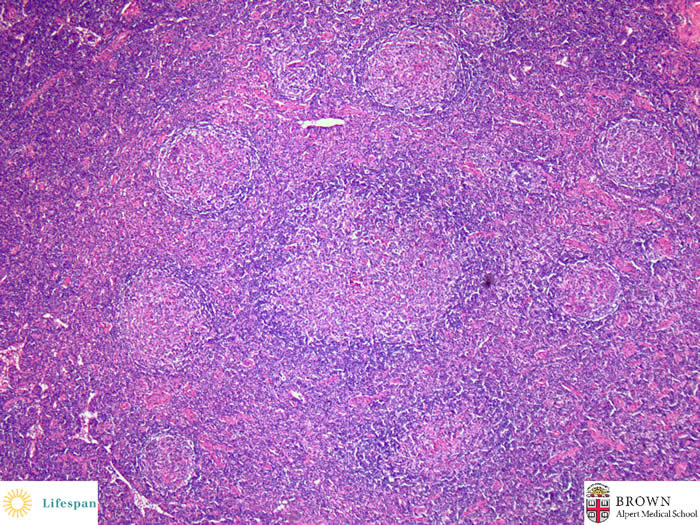
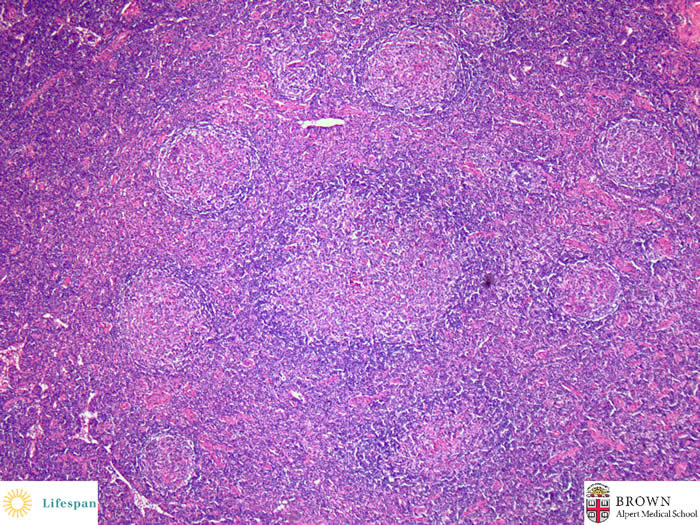
The germinal centers are at variant stages of regression. Mantle zones can be clearly identified.
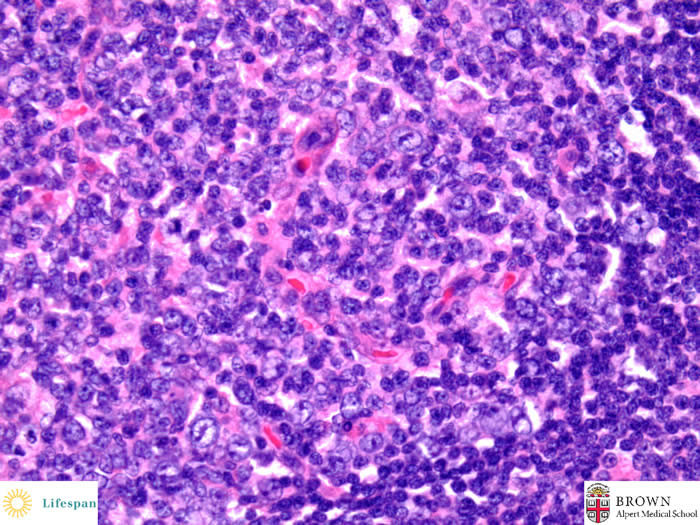
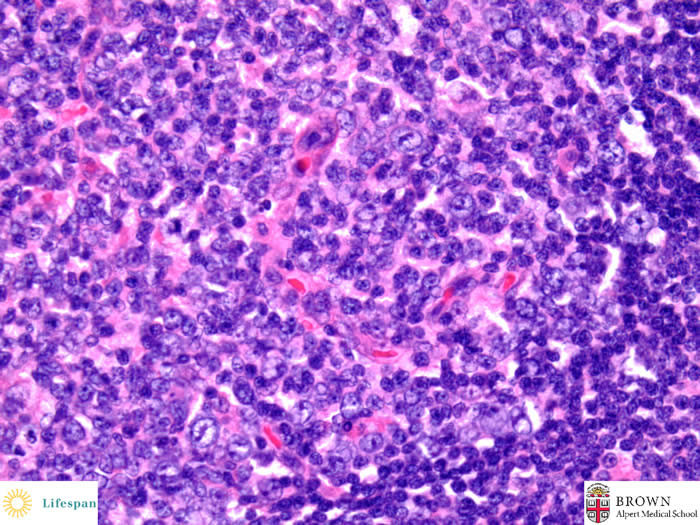
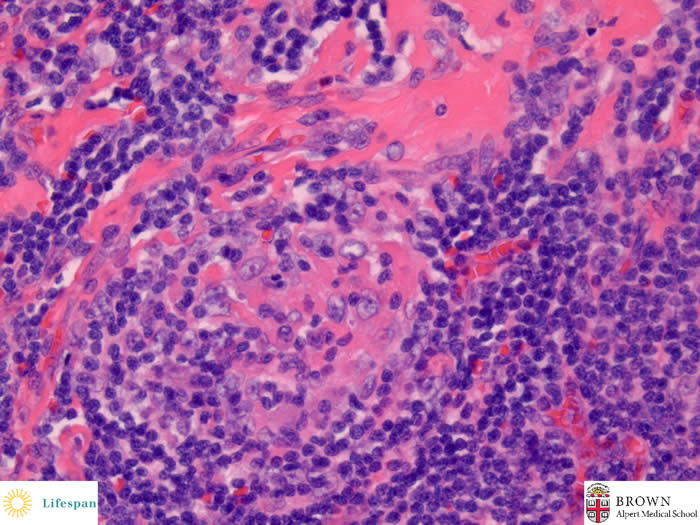
The germinal center contains numerous follicular dendritic cells, some hylinized blood vessels, and some large centrocytes.
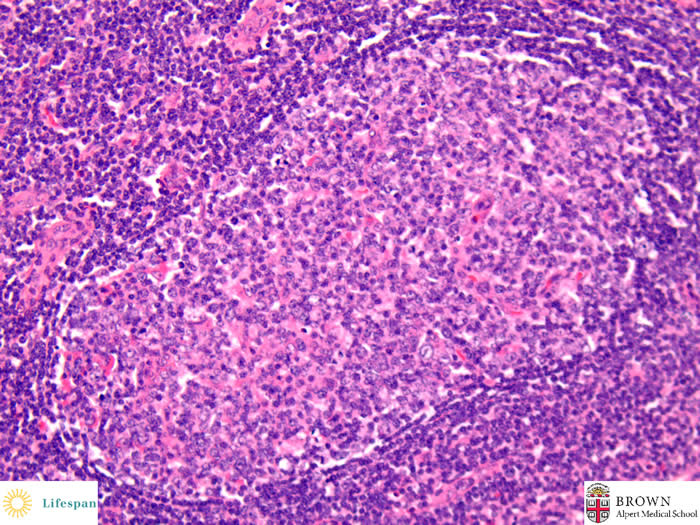
"Double germinal centers" exhibit two adjacent atrophic germinal centers encircled by a single mantle zone.
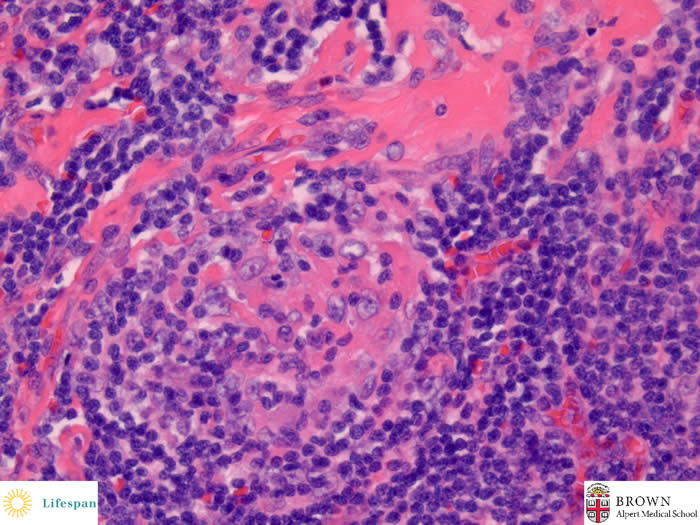
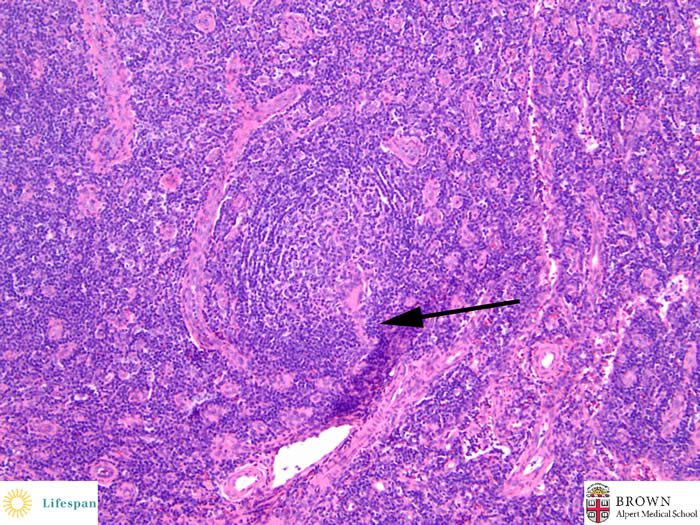
A hyalinized germinal center shows hyalinized area, dentritic cells and a mantle zone forming a somewhat "onion-skin" arrangement.
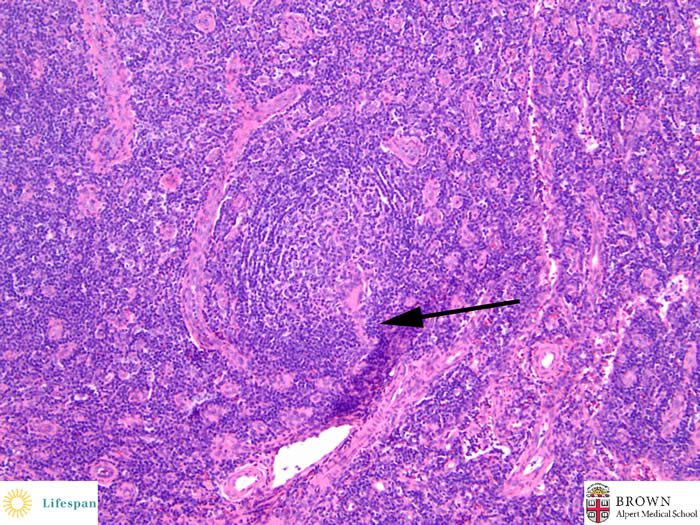
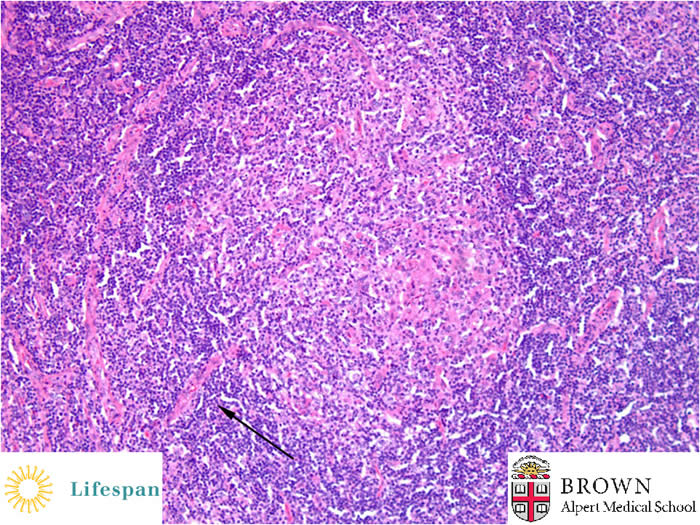
The above two geminal centers each have a central hyalinized vessel, giving a "lollipop" appearance.
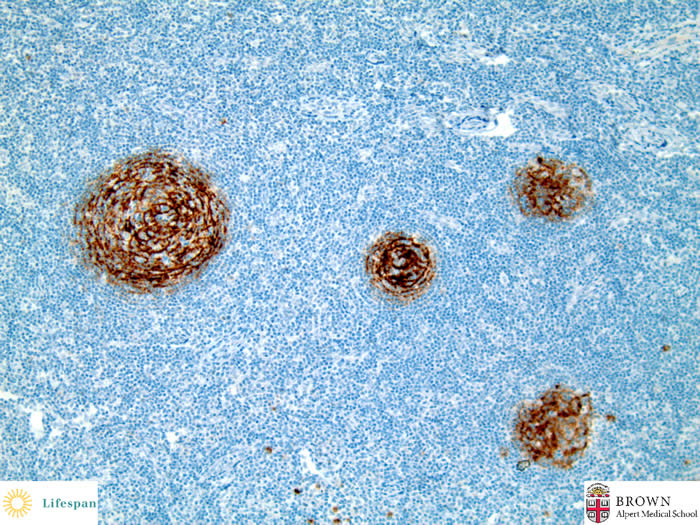
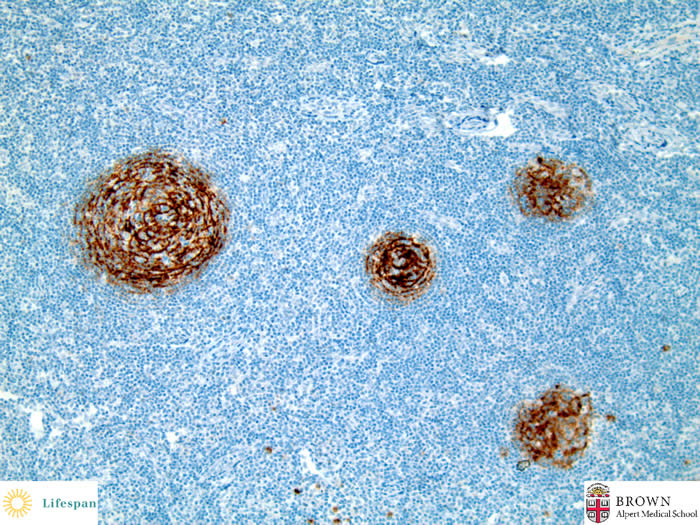
CD23 highlights follicular dendritic cell hyperplasia.
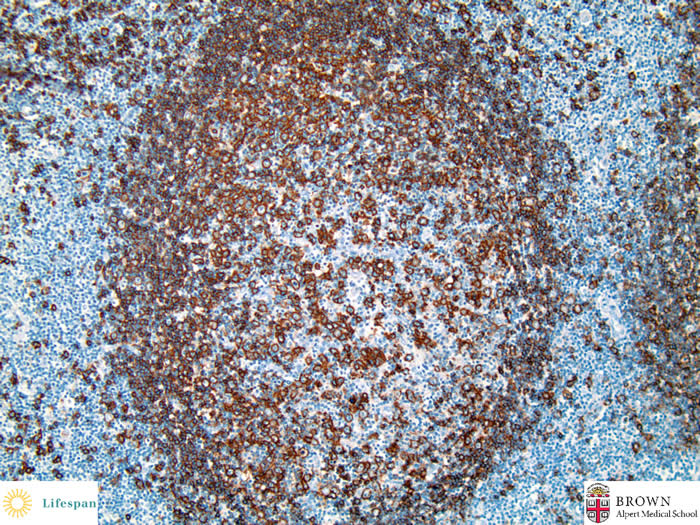
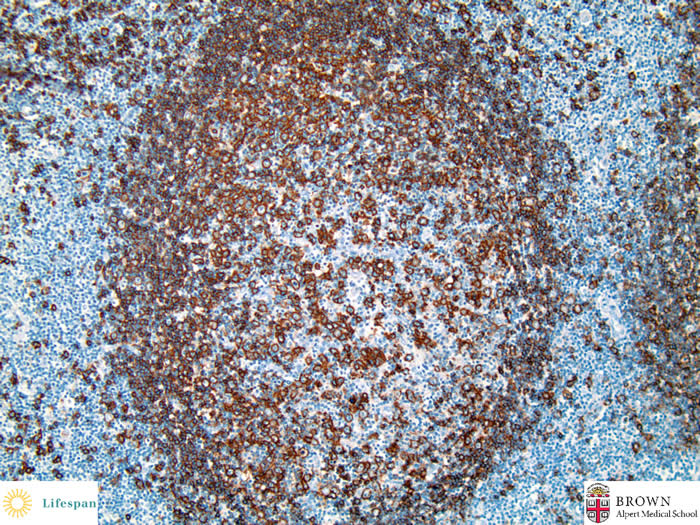
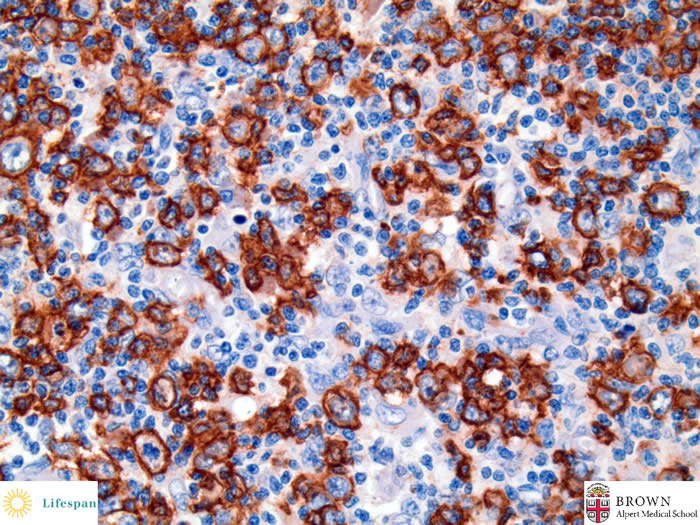
CD20 highlights a decreased B-cell population in germinal center.
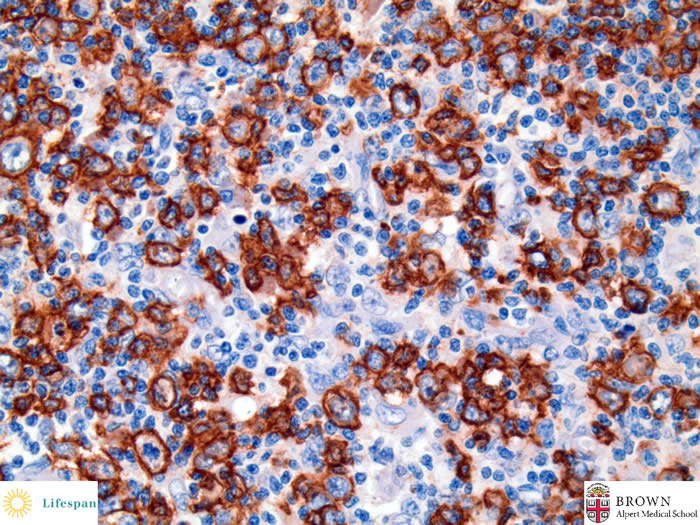
CD20 highlights some centrocytes in the germinal center.
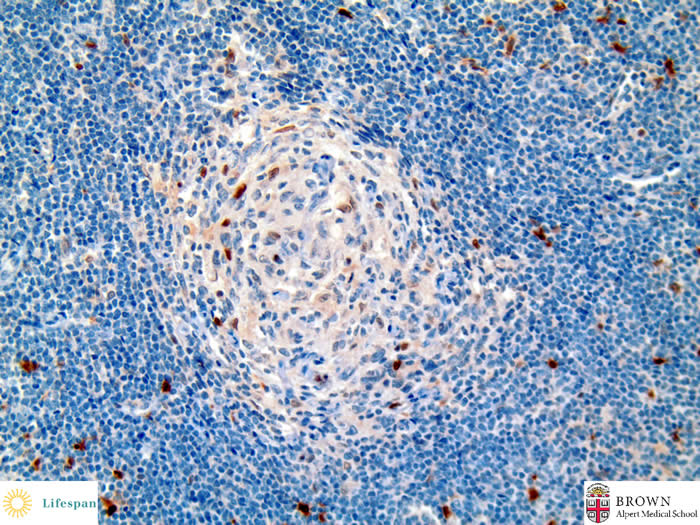
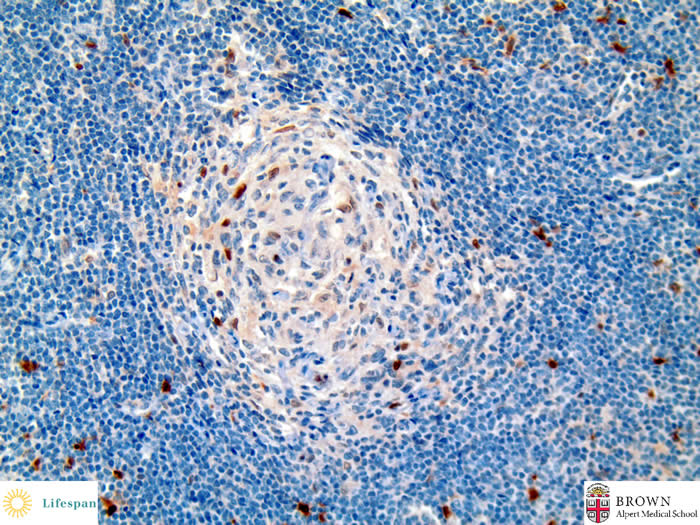
Another atrophic germinal center with decreased CD10(+) B-cells.
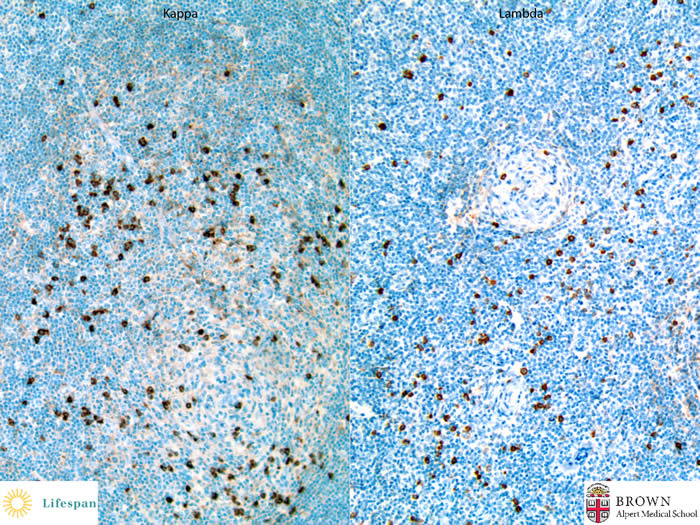
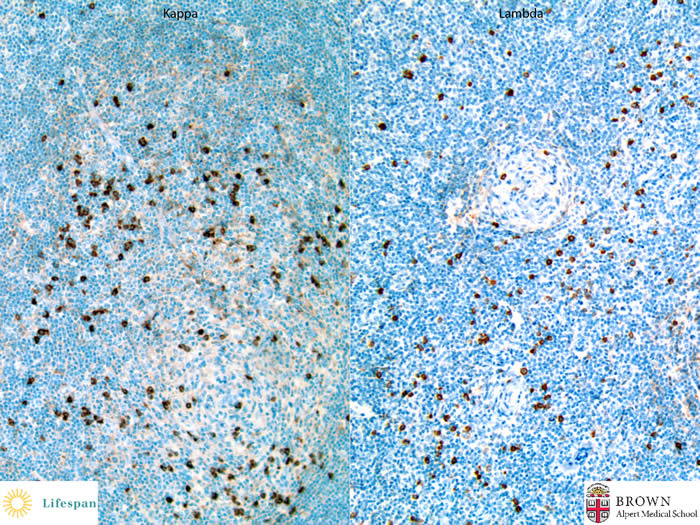
Kappa and Lambda light chain stainings confirmed absence of clonicity.
The final diagnosis is Castleman lymhadenopathy, hyaline-vascular variant.
Castleman's disease (CD), also called angiofollicular lymph node hyperplasia, comprises at least two distinct forms, unicentric (UCD) and multicentric (MCD). Its pathologic classification includes hyaline-vascular variant, plasma cell variant, mixed variant, and less frequent plasmablastic variant. Localized form was first described in 1956 by Benjamin Castleman. This form includes dominantly hyaline-vascular variant and a small amount of plasma cell variant and mixed variant. Multicentric Castleman's disease (MCD) is frequently associated with HHV-8 infection in immunodeficient or HIV-infected patients. MCD is more likely to be plasma cell variant or plasmablastic variant. Hematologic malignancy such as plasmablastic lymphoma arising from HHV-8 associated MCD has been reported. Kaposi's sarcoma, another HHV-8-related disease, is also highly correlated with MCD. UCD is also associated with non-Hodgkin lymphoma but to a much lesser extent.
The clinical course of MCD is very different from that of UCD. UCD in general can be cured by a simple surgical excision, while MCD has a much worse prognosis. Treatment of MCD is hampered by lack of knowledge of its etiology. Interleukin-6 (IL-6) and vascular epithelial growth factor (VEGF) have been shown to be involved in its pathogenesis. Anit-IL-6 antibody and anti-CD20 antibody are two new agents adding to variant combinations of chemotherapy and antiviral therapy.
Contributed by Shaolei Lu, MD
Previous | Return to Lymphatic Organ section
Home