Distributed May 31, 2002
For Immediate Release
News Service Contact: Scott Turner
Protein complex found to regulate first step in human blood clotting
Using human blood, Brown University scientists show that a complex of seven proteins is required for platelets to form the shape-changing filaments that begin a blood clot. Understanding this dynamic could lead to better treatments for abnormal clotting, which is the chief cause of stroke. The study appears in the June 15 issue of Blood.
PROVIDENCE, R.I. — Brown scientists have described a previously unknown but critical blood-clotting role for Arp2/3, a complex of seven proteins found in animal and plant cells.
Reporting in the June 15 issue of Blood, the scientists show that Arp2/3 complex is a cellular machine that drives a human blood platelet to change shape into a larger, more flattened form and begin the process of clotting. The link between what happens at the surface of a platelet and the mechanism of shape change within it has mystified scientists for decades. Arp2/3 has been found in yeast and a soil amoeba, as well as platelets.
“A major question for scientists has been how to control platelet shape change,” said the project’s senior researcher, Elaine Bearer, M.D., associate professor of pathology and laboratory medicine. “Understanding these molecular events could lead to better treatments for abnormal clotting.” Roughly 80 percent of strokes are caused by atypical clots that block blood flow.
Bearer and colleagues found that Arp2/3 complex is required for platelets to form the shape-changing filaments that begin the blood clotting process. The process of filament formation is called actin polymerization.
Actin filaments are fine threads composed of multiple subunits – polymers that line up like a sting of pop beads – which give structure to the cell, as well as drive shape changes, cell movements and other cellular processes. These filaments also participate in muscle contractions. The formation of filaments inside dividing cells also separates cytoplasm into the two daughter cells, so that each inherits the right amount of maternal material.
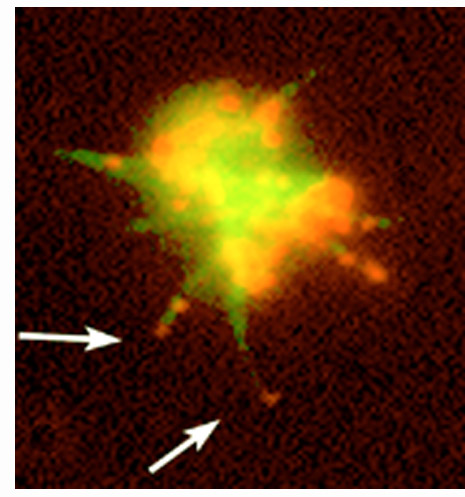
In these images, human blood platelets have been stained for actin filaments (green) and the Arp2/3 protein complex (red). In the first stage, top, the platelet is polymerizing actin into long arms that reach out and grab onto other cells. In the next stage, bottom, the platelet is spreading out. Note the Arp2/3 complex (red) at the tips and bases of the long arms (arrows) and at the outer edge of the spreading platelet. [Images: Elaine Bearer]
Since the first cell was observed under a microscope more than 200 years ago, scientists have sought to explain cellular shape change. Cell shape is used today for the pathologic diagnosis of tumors such as breast cancer. For 50 years, scientists have known that actin was required for shape change. Until now, they were unable to explain what drove actin to polymerize and form filaments.
 Polymerization of actin is an important first step in the process of platelet
clot formation. Platelets use these filaments to reach out and grab fibrin, the
major matrix material of clots, and other platelets, to form the clots.
Polymerization of actin is an important first step in the process of platelet
clot formation. Platelets use these filaments to reach out and grab fibrin, the
major matrix material of clots, and other platelets, to form the clots.
When a blood vessel is torn, molecules are released that bind to platelet surface receptors. This creates a cascade of events inside the first platelets that arrive at the wound, which change shape, sending out sticky arms into the blood flow to recruit other platelets that attach in an organized matrix to stop the bleeding and maintain the vessel.
Stroke, which results from abnormal clotting, is treated with blood thinning compounds to block platelets from forming clots. “A problem with this therapy is that it may completely stop platelet activity and a person may bleed to death,” Bearer said. “We would like to find a gentler way to block polymerization without this dangerous side effect.”
Cell biologists guessed that Arp2/3 complex played a role in nucleating new actin filaments because it did so in a test tube. Although many proteins play a similar role in test tubes, none has been found to be required in cells. Bearer and colleagues are the first to demonstrate that Arp2/3 complex plays a central role in nucleating actin filaments inside a cell.
“We think there are about 10 biochemical events between the cell and the polymerization process,” she said. “Each step triggers the next event in a pathway that culminates in polymerization. We’d like to learn how to control this process.”
Actin polymerization occurs in cells across the class of creatures called eukaryota. These include all animals, plants, fungi, algae and protozoa. Eukaryota share fundamental characteristics of cellular organization, biochemistry and molecular biology.
“Showing that the Arp2/3 complex is a major regulator in platelet actin dynamics leads us to believe that it plays this role in all cells, because all cells have shape-changing abilities that are required for many vital cell processes,” Bearer said. “Beyond representing a significant advance in the understanding of molecular events leading to platelet shape change, this work is likely to provide fundamental information about the principles and paradigms governing actin dynamics inside all cells.”
The Brown scientists developed new molecular-insertion technology – a model for testing the internal mechanisms of cells – to help them describe both the role of Arp2/3 as well as where it is located and activated during the stages of filament formation. The technology allowed researchers to “reach inside and tickle” the tiny platelets, without destroying them.
“It made it possible to manipulate the molecular composition of the platelet cytoplasm,” Bearer said. “This allowed us to investigate biochemical relationships between signaling pathways and the shape changes that occur in platelets but are common to all cells. The method provides a new model to test the effect of small molecules on signal pathways and shape changes in other human cells and other cell types.”
Besides Bearer, the research team included Zhi Li, lead author and doctoral student, and undergraduate Eric Kim. Both Li and Kim graduated in May 2002. Funding from the National Institutes of General Medical Sciences of the National Institutes of Health, a Salomon Research Award and the Brown University Undergraduate Teaching and Research Assistantships Program supported the work.
######