Course Directors:
|
Pathology |
Pathophysiology |
Pharmacology |
|
Kim Boekelheide & Calvin Oyer,
M.D. |
Douglas Burtt & Hank Wu, M.D.
|
Robert Patrick, Ph.D |
Questions 1 - 12:
An 82-year
old male with a 10-year history of a heart murmur presents to the hospital
emergency room with progressive shortness of breath of 24 hours duration.
On
examination, blood pressure is 110/90, pulse is 125 and irregularly irregular,
respirations are 28 and temperature is normal
Neck exam
reveals 10 cm jugular venous distension and delayed carotid upstrokes.
Chest
exam reveals a late-peaking systolic murmur at the base, radiating to the neck,
with a single second heart sound.
Chest
X-ray reveals pulmonary edema.
1. Which valvular abnormality does this patient
most likely have?
A) Hypertrophic Cardiomyopathy
with outflow tract obstruction
B) Aortic stenosis
C) Aortic insufficiency
D) Mitral stenosis
E) Mitral insufficiency
This patient’s electrocardiographic rhythm strip is shown below:
2. This patient’s heart rhythm irregularity is
most likely due to:
A) frequent atrial premature
contractions
B) multifocal atrial tachycardia
C) atrial fibrillation
D) frequent ventricular
premature contractions
E) ventricular tachycardia
3. This
patient’s heart rhythm may cause all of the following, except:
A) predisposition to
thrombo-embolism originating in the left atrium
B) reduced cardiac output due
to loss of the “atrial kick”
C) reduced stroke volume due to
increased heart rate
D) predisposition to
development of sudden death with ventricular fibrillation
E) variation in intensity of
the murmur from beat to beat
![]()
4. During the course of treatment of this
patient’s arrhythmia, Digoxin administration is considered.
Digoxin increases cardiac intracellular free calcium
levels via:
A) Stimulation of calcium
release from the sarcoplasmic reticulum
B)
Inhibition of adenylyl cyclase
activity
C)
Inhibition of Na+-K+ ATPase activity
D)
Stimulation of voltage-dependent calcium channels
E) Increasing the affinity of norepinephrine
for cardiac b-receptors
5. Which of the following sets of pressures was most
likely found on this patient at the time of cardiac catheterization (where RA =
right atrial pressure, PA = pulmonary artery pressure, PCW = pulmonary
capillary wedge pressure,
|
Units =
mmHg |
RA |
PA |
PCW |
|
Ao |
|
A) |
5 |
20/10 |
10 |
110/10 |
110/90 |
|
B) |
10 |
40/20 |
20 |
110/5 |
110/90 |
|
C) |
10 |
70/30 |
20 |
110/5 |
110/90 |
|
D) |
10 |
50/30 |
30 |
160/30 |
110/90 |
|
E) |
15 |
50/30 |
30 |
110/30 |
110/90 |
6. At which point on the following diastolic pressure/volume curves would this patient most likely be? (A, B, C, or D?)
7.
Treating this patient with a diuretic would cause the following change:
A) the patient would move from
the upper curve to a new curve, displaced down and to the right
B) the patient would move from
the lower curve to an upper curve, at the same vertical position
C) the patient would stay on
the same curve and move up and to the right
D) the patient would stay on
the same curve and move down and to the left
E)
the patient would move from the upper curve to a new curve, displaced
upwards and to the left
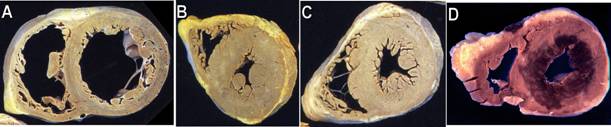
8. The clinical history in this case is most
consistent with which of the following gross images of a heart:
![]()
Questions 9 & 10 pertain to the following series of pressure-volume loops,
which was generated in the same patient.
9. What pharmacologic maneuver might cause the patient’s curve to change from curve 3 to curve 1:
A) Administration of an afterload reducing agent
B) Administration
of a diuretic
C) Administration
of an ACE-inhibitor
D) Administration
of a positive inotrope
E) Administration
of nesiritide (B-type natriuretic peptide)
10. All of the following effects would occur in changing the patient’s curve from
curve 3 to curve 1, except:
A) End-diastolic volume would be reduced
B) Stroke volume would be increased
C) Systolic blood pressure would be reduced
D) Diastolic blood pressure would be reduced
E) At the same heart rate, cardiac output would be increased
11. Which of the following heart structures is least likely to
be increased in number in this patient?
![]()
A) Myocytes
B) Interstitial fibroblasts
C) Mitochondria
D) Sarcomeres
E) Myocyte nuclei
12. At autopsy, myocardial hypertrophy is assessed most
accurately by the:
![]()
A) Left ventricular wall thickness
B) Diameter of the left ventricle at a mid-septal level
C) Measurement of heart size from a chest x-ray
D) Weight of the heart
E) Microscopic examination of the left ventricular myocardium
Questions 13 – 18:
A 74
year-old female with long-standing hypertension presents to the hospital with
mid-sternal chest pressure and dyspnea. She is too ill to give an adequate
history. Pertinent physical findings include:
Heart rate: 110,
regular; Blood Pressure: 180/90;
Respirations: 24
Neck: 10 cm jugular venous distension; normal
carotid upstrokes
Chest: rales are audible ½ of the
way up both lung fields
Heart: Rapid,
regular S1 and S2 with a III/VI systolic murmur at the
left sternal border and apex, radiating to the back
Extremities: cool; no edema,
cyanosis or clubbing
The electrocardiogram reveals
sinus tachycardia with ST segment elevation and Q waves in several leads.
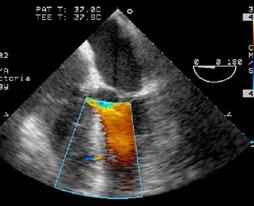
A bedside echocardiogram is performed on the patient
and is shown below:
13.
The initiating event for this patient’s illness most likely occurred:
![]()
A) Within the last hour
B) Within the last 12 hours
C) About 1 day ago
D) About 3-10 days ago
E) About 1 month ago
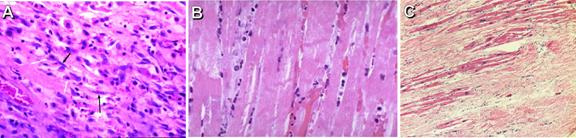
14. Which
of the following microscopic images of the patient’s injured heart muscle at
the time of visiting the ER is most consistent with the clinical history?
![]()
15. Treatment of the patient at this time might
include all of the following, except:
A) administration of
thrombolytic therapy
B) emergency cardiac
catheterization
C) placement of an intra-aortic
balloon pump
D) surgical consultation for
possible open-heart surgery
E) vasodilator drugs to reduce afterload and augment forward cardiac output
16. All of the following statements about this
patient’s myocardial infarction are true, except:
A) the “ischemic cascade”
starting at the onset of her myocardial infarction includes diastolic
dysfunction, systolic dysfunction, EKG changes and chest pain
B) the myocardial infarction
proceeds in a “wavefront” manner, proceeding from epicardium to endocardium
C) systolic dysfunction caused
by the infarction may lead to further ischemia by decreasing coronary perfusion
pressure
D) diastolic dysfunction caused
by the infarction may lead to increased wall tension, increased
E) sympathetic stimulation due
to the pain of the infarction may increase myocardial oxygen demand (MVO2)
17.
As part of the treatment of this patient, the drug captopril is administered.
Indicate which of the following statements concerning captopril is/are correct:
![]()
A.
It reduces circulating levels of bradykinin
B.
It can produce a persistent dry cough
C.
It is an antagonist of an angiotensin II receptor
D.
A and B
E.
B and C
18.
As part of the treatment of this patient, a right heart catheterization is
performed. Which right heart catheterization results are most likely from this
patient?
|
Answer |
PCW mean pressure |
PCW V wave pressure |
RA oxygen saturation |
PA oxygen saturation |
|
A |
30 |
30 |
60% |
85% |
|
B |
10 |
10 |
80% |
80% |
|
C |
30 |
60 |
70% |
70% |
|
D |
20 |
20 |
80% |
60% |
|
E |
30 |
30 |
85% |
85% |

Questions 19 – 24:
A
thirty-five year old male Egyptian immigrant presents to the medical clinic for
a pre-employment physical. He states that he had no prior illnesses but has
been having some dyspnea on climbing stairs recently. On physical examination,
his main finding is that of a loud first heart sound, a high-pitched sound
immediately after S2, and a low-pitched
diastolic murmur during diastole.
19. As a teenager, this patient
experienced an acute, severe sore throat that resolved after about a week. A
month or two later, the patient experienced a period of poor exercise
tolerance, shortness of breath, and malaise. The likely inciting event in this
patient’s illness is:
![]()
A) An infective endocarditis
B) A transmural myocardial
infarction
C) Chronic pulmonary emboli
D) An autoimmune response
E) None of the above
20. If an endomyocardial
biopsy were performed on this patient at the time of clinical cardiovascular
illness later in adulthood, the most likely finding would be:
![]()
A) Increased fibrosis
B) Acute inflammation
C) Anitschkow cells
D) Caterpillar cells
E) Fibrinoid necrosis
![]()
21. The
most commonly involved valves in this patient’s disease, from most common to
least common are:
A) mitral, tricuspid, aortic pulmonary
B) aortic, mitral, tricuspid, pulmonary
C) aortic, pulmonary, tricuspid, mitral
D) mitral, aortic, tricuspid, pulmonary
E) pulmonary, tricuspid, mitral, aortic
22.
This patient is likely to have all of the following anatomical or physiological
findings, except:
A) a normal left ventricle
B) a dilated left atrium
C) thinned and elongated chordae
tendinae
D) doming of the mitral valve leaflets
E) mildly elevated pulmonary artery pressures
23. The predominant physiological
abnormality in this patient is:
A) impaired emptying of the left ventricle
B) impaired filling of the left ventricle
C) volume overload of the left ventricle
D) pressure overload of the left ventricle
E) diastolic left ventricular dysfunction
24. Cardiac catheterization of this patient might demonstrate a gradient
between which two pressures:
A) Left ventricular and
pulmonary capillary wedge pressure during diastole
B) Ascending aortic pressure
and left ventricular pressure during systole
C) Right atrial and right
ventricular pressure during diastole
D) Right ventricular and
pulmonary artery pressure during systole
E) Left ventricular and left
atrial pressure during systole
Questions
25 – 28:
A
48 year old patient with history of treated tuberculosis presents to the
doctor’s office with progressive fatigue, dyspnea on exertion, abdominal
swelling and ankle edema.
Physical
findings include:
Pulse: 110 and regular; BP:
100/70 without a pulsus paradoxus;
Resp: 20
Elevated neck veins, which elevate further with
inspiration
Minimal rales at the lung bases
An early diastolic sound shortly after S2
Distension of the abdomen consistent with ascites, with hepatomegaly
2 – 3+ pitting edema of the ankles
25.
The LEAST likely cause of this patient’s illness is:
![]()
A) a prior viral infection
B) a prior bacterial infection
C) a prior mycobacterial
infection
D) a prior fungal infection
26. Cardiac catheterization findings on this patient
are likely to include all of the following, except:
A) A blunted y-descent due to
impaired rapid ventricular filling of the RV
B) Elevated and equalized
diastolic intra-cardiac pressures
C) A “dip and plateau” during
rapid ventricular filling of the RV
D) A prominent y-descent due to
rapid RA emptying
E) An inspiratory rise in
jugular venous pressure
27. This patient’s current clinical condition would
be likely to:
A) respond to treatment with
non-steroidal anti-inflammatory drugs
B) be accompanied by a fever
C) respond to pericardiocentesis
D) be associated with fusion of
the pericardial tissue layers
E) manifest an accentuated
decrease in systolic blood pressure with inspiration
28. Of the following right atrial pressure tracings,
which most closely resembles this patient’s:

Questions 29 – 40:
A
patient presents to the hospital with an acute anterior myocardial infarction
associated with congestive heart failure. A right heart catheterization is
performed in the CCU.
This
patient’s Frank Starling curve is represented below as the lower of the two
curves below.
Please answer the
next TRUE or FALSE questions based on this diagram (A = TRUE
; B = FALSE).
29. This patient’s
prognosis is better if he is on point A rather than point B on the curve.
30. This patient
can be moved from point B to point C by administering fluids.
31. This patient
can be moved from point A to point B by administering a positive inotrope.
32. Patients
falling into Quadrant IV have a mortality rate of less than 30 percent.
33. Patients
falling into Quadrant III usually have clear lungs and low blood pressure.
34. Patients in
Quadrant II have the worst prognosis of all.
35.
The Fick Method of determining this patient’s cardiac output predicts all of
the following, except:
A) An increase in mixed venous
oxygen saturation suggests an increase in cardiac output
B) A decrease in oxygen
consumption suggests an increase in cardiac output
C) The cardiac output can be
estimated using three parameters: the oxygen consumption, the arterial oxygen
saturation and the mixed venous oxygen saturation
D) The calculation of the
cardiac output using the Fick method is independent of the ability of the lungs
to oxygenate the blood
E) An increase in cardiac
output coincides with a lower A-V O2 saturation difference
36. As part of this
patient’s treatment you plan to use a positive inotropic
agent. Which of the following inotropic
agents also has significant vasodilating properties:
A)
Digoxin
![]()
B) Dopamine
C) Epinephrine
D) Milrinone
E) Norepinephrine
37.
With regard to the pharmacotherapy of patients with congestive heart failure,
which of the following drug-pairs DO NOT exhibit potentiation
of action when used in combination to improve symptoms in congestive heart
failure:
![]()
A) Angiotensin converting
enzyme inhibitors and loop diuretics
B) Hydralazine and isosorbide (nitrates)
C) Metolazone (a thiazide)
and loop diuretics
D) Beta blockers and dobutamine
E) All of the above
38. The mechanisms of action by which angiotensin
converting enzyme inhibitors (ACE inhibitors) may be effective in the treatment
of congestive heart failure are:
![]()
A) Afterload reduction by
inducing vasodilation
B) Preload reduction by
promoting diuresis
C) Increase in myocardial
contractility through neurohormonal antagonism
D) a. and b.
E) b. and c.
39. Several weeks after his myocardial infarction
the patient undergoes echocardiography which demonstrates an ejection fraction
of 30% (normal = 55 – 70%). You want to
make sure that the medications you are planning to prescribe have proven
efficacy on prolonging the survival
of patients with heart failure. Examples
of such medications include:
![]()
A) Angiotensin converting
enzyme inhibitors
B) Beta blockers
C) Phosphodiesterase inhibitors
D) a. and b.
E) a. and c.
40. After several years, this patient has been
using digoxin for the treatment of his heart failure
without any problems. His doctor
recently told him that his renal function has gotten progressively worse, so
the digoxin levels as well as serum electrolytes have
to be monitored more closely to avoid the development of digoxin
toxicity. Please point out the set of
electrolyte abnormalities that would predispose the patient to develop digoxin toxicity:
![]()
A) Hypermagnesemia, hypokalemia
and hypercalcemia
B) Hypomagnesemia, hypokalemia
and hypercalcemia
C) Hypermagnesemia, hyperkalemia
and hypercalcemia
D) Hypermagnesemia, hypokalemia
and hypocalcemia
E) Hypomagnesemia, hypokalemia
and hypocalcemia
Questions 41 – 67 are all Pharmacology questions:
41.
A patient presents with excessive salivation together with episodes of vomiting
and shows signs of general skeletal muscle weakness. Untreated, the patient suffers clonic convulsions and requires artificial
respiration. Poisoning with which one of
the following should be suspected?:
![]()
A. Pralidoxime
B.
Atropine
C. Tubocurare
D. Muscarine
E.
Nicotine
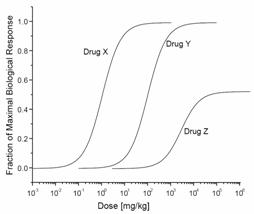 42. The figure below depicts
the dose-response curves for drug X, Y, and Z.
A comparison of the curves shows that drug X:
42. The figure below depicts
the dose-response curves for drug X, Y, and Z.
A comparison of the curves shows that drug X:
A.
has greater efficacy than drug Y
B.
has less efficacy than drug Y
C.
has the same potency as drug Y
D.
is more potent than drug Y
E.
is safer than drug Y and drug Z
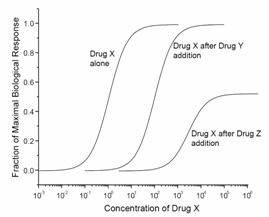 43. The figure below depicts
the dose-response curve when drug X is given alone and when it is given in the
presence of a fixed dose of either drug Y or drug Z. Neither drug Y nor drug Z
elicit any response when given alone.
Drug Y in this figure is a:
43. The figure below depicts
the dose-response curve when drug X is given alone and when it is given in the
presence of a fixed dose of either drug Y or drug Z. Neither drug Y nor drug Z
elicit any response when given alone.
Drug Y in this figure is a:
A.
Competitive antagonist
B. Full agonist
C. Noncompetitive antagonist
D. Partial agonist
E. Irreversible competitive antagonist
44.
For increasing heart rate: Drug A has an ED50 of 8 mg/kg
and Drug B has an ED50 of 20 mg/kg. From this we can conclude that:
A.
Drug B is more potent compared to Drug A
B.
Drug B has a greater efficacy (maximal effect) compared to Drug A
C.
Drug A is a partial agonist
D.
Drug B is a partial agonist
E.
None of the above
![]() All Pharmacology
All Pharmacology ![]()
45. Drug C has an ED50 of 20 mg/kg and a TD50 of 4 mg/kg. Indicate the Therapeutic Index (TI)
of Drug C:
A.
80
B.
20
C.
5
D.
0.20
E.
None of the above
46. An ophthalmologist instills a 2.5% solution
of phenylephrine into a patient’s eyes before
examining them. The drug causes mydriasis by:
A.
Decreasing the level of cyclic adenosine monophosphate
(cAMP)
B.
Increasing the levels of IP3 and diacylglycerol (DAG)
C.
Facilitating the binding of ATP and the opening of a K-channel
D.
Increasing the levels of cAMP
E.
Increasing the synthesis of proteins through gene expression mechanisms
47. An example of a direct agonist of the
cholinergic receptor located at the neuromuscular junction (skeletal muscle):
A.
Atropine
B. Clonidine
C.
Nicotine
D. Prazosin
E.
Atenolol
48. The main neurotransmitter utilized by the preganglionic neurons of the sympathetic nervous system is:
A.
Dopamine
B.
Acetylcholine
C.
Epinephrine
D.
Norepinephrine
E. Choline
49. Indicate which of the following statements
concerning cholinergic receptors are CORRECT:
A.
The main targets of postganglionic parasympathetic innervation
of the heart are nicotinic receptors
B. Muscarinic receptors are G-protein coupled
receptors
C.
Blockade of muscarinic receptors in the eye leads to
pupil dilation
D.
A and B
E.
B and C
50. Indicate which of the following statements
concerning catecholamines is/are CORRECT:
A.
Catecholamine stimulation of b2 receptors on vascular smooth
muscle produces vasoconstriction
B. Propranolol can precipitate a dangerous bronchoconstriction
in an asthmatic patient
C.
In catecholamine neurons, dopamine is synthesized from epinephrine
D.
A and B
E.
B and C
![]() All Pharmacology
All Pharmacology ![]()
51. Inhibition of acetylcholinesterase
activity, as by nerve gases, is associated with all of the following, EXCEPT:
A.
Involuntary urination
B. Bradycardia
C.
Excessive tear formation in the eyes
D.
Constipation
E.
Excessive saliva production
------------------------------------------
Questions
52 – 55 – match each question with the correct drug(s):