BIO-MED 350
COMBINED CARDIAC PATHOPHYSIOLOGY,
PHARMACOLOGY & PATHOLOGY EXAM
2006
Questions 1 - 9:
A
54 year old male presents to the hospital with progressive symptoms of
shortness of breath. Physical
examination reveals a systolic heart murmur and lung findings consistent with
congestive heart failure. An echocardiogram is performed and reveals a significant
cardiac structural abnormality.
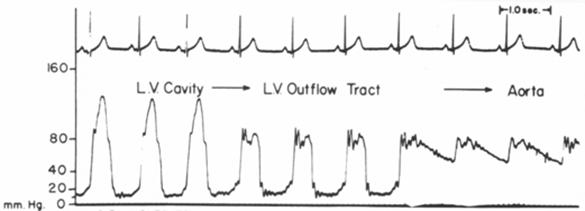
For further diagnosis, a
cardiac catheterization is performed, and the following tracing is obtained
while pulling back the catheter from the left ventricular apex to the aorta:
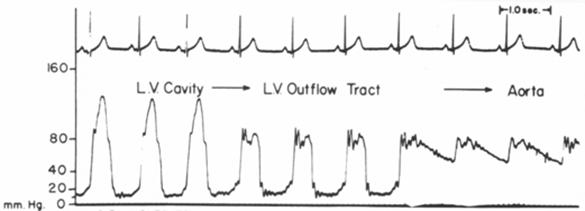
1. This patient’s cardiac structural abnormality
most likely represents:
A)
mitral stenosis
B)
aortic stenosis
C)
hypertrophic
cardiomyopathy with LV outflow obstruction
D)
pulmonic
stenosis
E)
coarctation of
the aorta
Questions 2 - 7:
Please
indicate (true or false), whether each of the following is associated with this
patient’s condition:
2. Impaired systolic
LV function
3. Impaired diastolic
LV function
4. Increased risk of sudden cardiac
death
5. Mitral regurgitation
6. Delayed and diminished carotid
upstrokes
7. Reduction of heart murmur intensity
with standing up
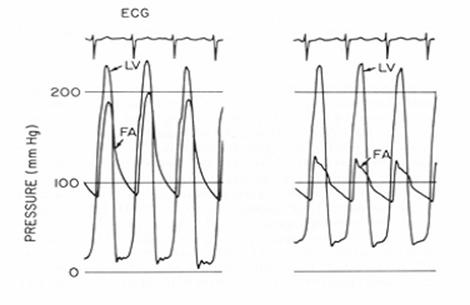
The following sets of tracings are obtained before and after an
intervention:
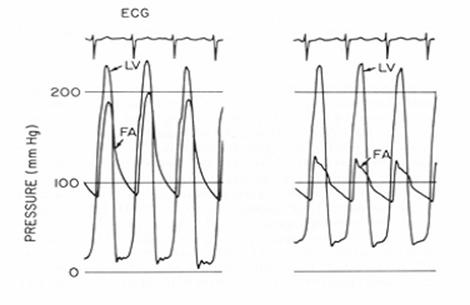
BEFORE AFTER
8. The most likely
intervention to cause this change in pressures was:
A) Valsalva
maneuver
B) Squatting
C) Passive
leg raising
D) Volume infusion
with normal saline
This
same patient develops palpitations and lightheadedness. An EKG reveals rapid
atrial fibrillation with a ventricular response rate of 130 beats per minute.
9.
All of the following medications may help slow his heart rate, except:
A)
Amlodipine
B)
Diltiazem
C)
Verapamil
D)
Digoxin
E)
A beta-blocker
*************************************************************************
10.
The best drug to use for rapidly controlling the ventricular response in a
patient with new onset atrial fibrillation is:
A) digoxin
B) amiodarone
C) verapamil
D) adenosine
E) flecainide
11. Which of the following statements best describes the
normal conduction of electrical impulses through the AV node?
A) Transmembrane
calcium currents are responsible for activation of AV nodal cells, resulting in
relatively slow conduction, in comparison to working ventricular myocytes.
B) Transmembrane
sodium currents are responsible for activation of AV nodal cells, resulting in
relatively slow conduction, in comparison to working ventricular myocytes.
C) Parasympathetic
stimulation has little effect during the resting state on the behavior of AV
nodal cells
D) Sympathetic
stimulation has little effect during the resting state on the behavior of AV
nodal cells
12. The mechanism responsible for the majority of pathologic
clinical cardiac arrhythmias is:
A) Intramyocardial reentry due to functionally-based circuits.
B) Intramyocardial
reentry due to anatomically-based circuits.
C) Triggered
activity due to delayed afterdepolarizations.
D) Triggered
activity due to early afterdepolarizations.
E) Abnormal
automaticity
13. The major antiarrhythmic actions of digitalis are due
to:
A) Sympathetic
blockade
B) Inhibition
of the Na/K ATPase pump
C) Parasympathomimetic
actions
D) Improvement
in ventricular function resulting from its positive inotropic effects.
14. Which of the following agents should never be used to
treat atrial fibrillation in a 50 year old man who experienced myocardial
infarction 5 years previously:
A) Digitalis
B) Verapamil
C) Dofetilide
D) Flecainide
15. Development of a prolonged QT interval and torsade de
pointes is unlikely to occur with which of the following antiarrhythmic agents?
A) Procainamide
B) Amiodarone
C) Quinidine
D) Verapamil
**************************************************************
Questions 16 - 22:
A 75 year-old Middle Eastern
female presents to the hospital with progressive fatigue, abdominal swelling
and ankle edema. She has gained over 25 pounds over the last month, and
has been sleeping in a recliner chair.
The patient relates a remote history of
tuberculosis, which has been treated and “eradicated”.
On examination, her jugular veins are
distended, her lung fields are clear, and she has evidence of ascites and
peripheral edema.
Right heart catheterization is performed and
the following tracings are obtained (RA = right atrium; RV = right ventricle;
LV = left ventricle):


The
patient is likely to manifest each of the following features:
( A/True or
B/False ):
16. Kussmaul’s
sign
17. Pulsus
paradoxus
18. Equalization of diastolic
pressures
19. Auscultatory
finding of a pericardial “Knock”
20. Reduced forward cardiac output
21. Calcification of the heart border
on Chest X-ray
22. Reduced left ventricular systolic
function
*********************************************************************************
Questions 23 - 31:
A forty five year old male with history of
hypertension, high cholesterol and cigarette smoking presents to the emergency
room with severe mid-sternal chest “heaviness”, radiating to his neck and arms,
of one hour’s duration.
An electrocardiogram reveals ST-segment
elevation in the inferior leads.
On examination, the patient’s pulse is slow,
50 beats per minute, and the blood pressure is mildly reduced, at 90/60 mm Hg.
23.
Causes of this patient’s bradycardia (slow heart rate) might include all of the
following, except:
A) a re-entry circuit within the left ventricle
B) sinus node
ischemia
C) A-V node
ischemia, causing Mobitz I (Wenckebach) 2nd degree block
D) Increased vagal
(parasympathetic) tone
E) A-V node
ischemia, causing 3rd degree AV block with a junctional escape rhythm
24. The most likely major contributing cause to this
patient’s low blood pressure at the present time is:
A) Acute mitral
regurgitation from papillary muscle rupture
B)
Acute right ventricular infarction, causing
decreased LV preload
C) Significant
left ventricular infarction, causing markedly reduced LV stroke volume
D) Acute
ventricular septal rupture
E) Pericardial
tamponade from LV free-wall rupture
25. All of the following statements about this
patient’s acute myocardial infarction are true, except:
A)
the “ischemic
cascade” starting at the onset of his myocardial infarction includes diastolic
dysfunction, systolic dysfunction, EKG changes and chest pain
B)
the myocardial infarction proceeds in a “wavefront”
manner, proceeding from epicardium to endocardium
C)
systolic
dysfunction caused by the infarction may lead to further ischemia by decreasing
coronary perfusion pressure
D)
diastolic
dysfunction caused by the infarction may lead to increased wall tension and
decreased oxygen delivery to the myocardium
E)
sympathetic
stimulation due to the pain of the infarction may increase myocardial oxygen
demand (MVO2)
Several
days after the patient’s initial myocardial infarction, the patient develops
worsening shortness of breath and is noted to have a new, harsh systolic
murmur. Right heart catheterization
reveals the following findings:
|
|
Oxygen Saturation
|
Pressure (mm Hg)
|
|
Right Atrium
|
70%
|
8
|
|
Right Ventricle
|
72%
|
40/8
|
|
Pulmonary Artery
|
71%
|
40/22
|
|
Pulmonary Capillary Wedge
|
|
25 mean
V-waves
to 50
|
26.
This patient’s echocardiogram might be expected to show:
A)
Acute mitral regurgitation
B)
Acute
ventricular septal defect
C)
Acute right
ventricular infarction
D)
Cardiac
tamponade
E)
Apical
LV aneurysm formation
27. Treatment of the patient at this time might
include all of the following, except:
A)
administration of thrombolytic therapy
B)
emergency
cardiac catheterization
C)
placement of an
intra-aortic balloon pump
D)
surgical
consultation for possible open-heart surgery
E)
vasodilatory drugs to
augment forward cardiac output
28.
Intra aortic balloon pump placement may do all of the following,
except:
A)
Reduce
LV afterload
B)
Reduce
LV preload
C)
Increase
coronary blood flow
D)
Reduce
myocardial oxygen demand
E)
Increase
cardiac output
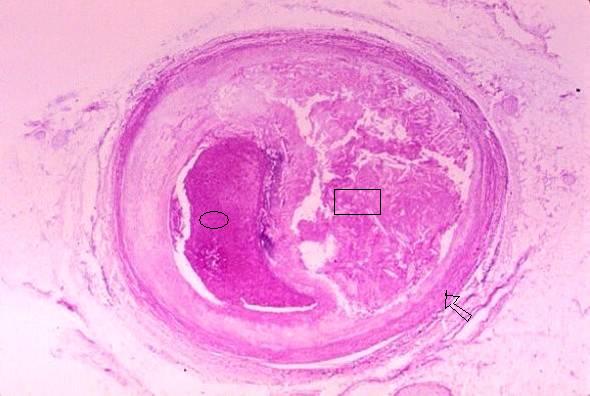
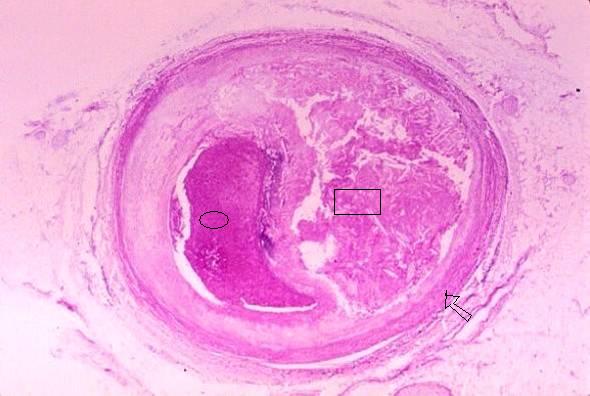
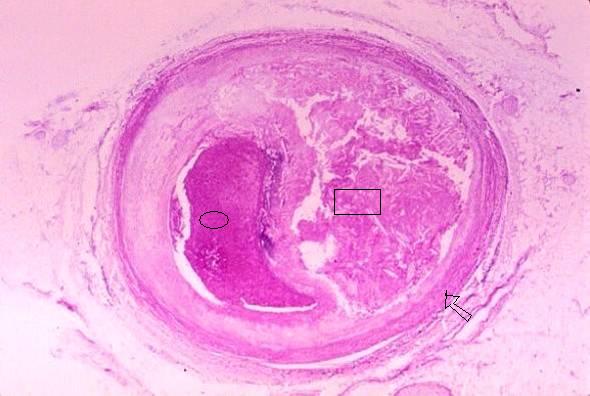
Unfortunately,
despite your team’s best medical efforts, the above patient dies of congestive
heart failure. The following photograph shows a cross-section of the patient’s
right coronary artery. Please answer the questions below the photo.
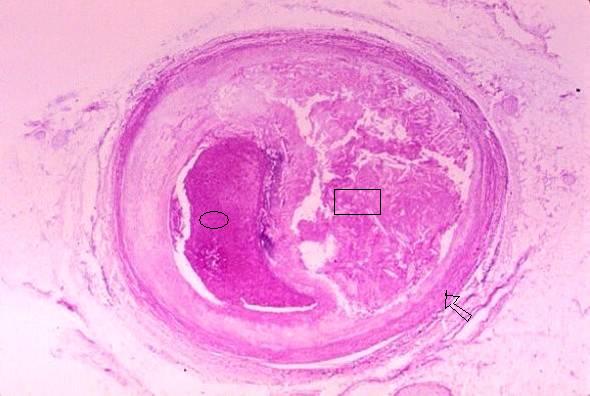
29.
The object indicated by the oval is:
A)
the central
core of an atherosclerotic plaque
B)
a thrombus occluding the lumen of the artery
C)
a large calcium
deposit in a thickened intima
30.
The rectangle is positioned in:
A)
a thrombus
occluding the lumen of the artery
B)
a large calcium
deposit
C)
the central core of an atherosclerotic plaque
31.
The arrow points to:
A)
the media
B)
the intima,
which in that location is uninvolved
C)
the adventitia
Questions 32 - 37:
A patient presents to the hospital with an acute anterior
myocardial infarction associated with congestive heart failure. A right heart
catheterization is performed in the CCU.
This patient’s Frank Starling curve is represented below as
the lower of the two curves below.
Please answer the next TRUE or FALSE questions based on this
diagram (A = TRUE; B = FALSE).
32. This patient’s prognosis is worse if he is on point A
rather than point B on the curve.
33. This patient can be moved from point B to point C by
administering fluids.
34. This patient can be moved from point A to point B by
administering fluids.
35. Patients falling into Quadrant IV have a mortality rate
of less than 30 percent.
36. Patients falling into Quadrant III usually have pulmonary
congestion and a normal blood pressure.
37. Patients in Quadrant II have the worst prognosis of all.
Questions 38 - 40:
A 48-year-old Saudi Arabian female with a history of
rheumatic fever at age 20 presents to the office with progressive fatigue and
dyspnea on exertion. Physical examination reveals:
Heart
rate: 90, regular; Blood Pressure: 120/70;
Respirations: 18
Neck: 8 cm JVD with prominent jugular V-waves;
normal carotid upstrokes
Chest: Fine
rales at the bases
Cor:
Prominent S1, increased pulmonic component of S2; high-pitched snap
shortly after S2; soft, II/VI systolic blowing murmur at the left sternal
border, increasing with inspiration; soft diastolic rumble with pre-systolic
accentuation
Extremities:
trace edema; no cyanosis
38. One would expect that this patient’s valvular
abnormalities would include:
A)
Mitral
stenosis and tricuspid insufficiency
B)
Aortic
insufficiency and mitral regurgitation
C)
Aortic
stenosis and mitral regurgitation
D)
Mitral
stenosis and aortic insufficiency
E)
Hypertrophic
cardiomyopathy with outflow tract obstruction
39. On echocardiography, one would expect that this
patient’s left ventricle would demonstrate:
A)
Concentric
left ventricular hypertrophy
B)
Cavity
dilation and global left ventricular hypokinesis
C)
Normal
cavity size and normal left ventricular function
D)
Discrete
sub-aortic septal hypertrophy
E)
Normal left ventricular size, with severe
global hypokinesis
40. Cardiac catheterization might demonstrate a gradient
between which two pressures:
A)
Left
ventricular and pulmonary capillary wedge pressure during diastole
B)
Ascending aortic pressure and left ventricular pressure during systole
C)
Right
atrial and right ventricular pressure during diastole
D)
Right
ventricular and pulmonary artery pressure during systole
PHARMACOLOGY QUESTIONS:
41. An 82 year-old woman presents to the Emergency Room
with a history of new-onset syncope. Upon arrival, she is awake and oriented
and has a small laceration on her forehead. Her blood pressure is 165/86 mmHg
and her heart rate is 43 beats /minute. She is receiving unknown medications
for chest discomfort provoked by exertion and relieved by rest. Which of the
following combinations of drugs would most likely explain this patient’s
presentation?
A)
Diltiazem, nitroglycerin spray
B)
Verapamil, Atenolol, Isosorbide
dinitrate
C)
Nifedipine, Isosorbide Mononitrate
patch
D)
Amlodipine, sublingual nitroglycerin
42. Indicate which of the choices below describes the effects
of a competitive antagonist on drug ED50 and efficacy.
A)
A
decrease in ED50 with no change in efficacy
B)
A
decrease in ED50 and a decrease in efficacy
C)
No
change in ED50 and a decrease in efficacy
D)
An
increase in ED50 and no change in efficacy
E)
An
increase in ED50 and an increase in efficacy
43. An example of a ligand-gated receptor:
A)
Muscarinic
receptor
B)
b-1 receptor
C)
Nicotinic
receptor
D)
b-2 receptor
E)
a-1 receptor
44. Indicate which of the drugs below has the greatest potency for
producing ganglionic blockade:
A)
Trimethaphan
B)
Propranolol
C)
Atropine
D)
Pralidoxime
(2-PAM)
E)
Acetylcholine
45. Indicate which of the agents below is used most often to
help diagnose myasthenia gravis:
A)
Atropine
B)
Trimethaphan
C)
Pancuronium
D)
Mecamylamine
E)
Edrophonium
46. All of the following statements regarding neuromuscular
blockers are correct EXCEPT:
A)
Atracurium is a competitive blocker
B)
Succinycholine-induced blockade can
be reversed by acetylcholinesterase inhibitors
C)
Anesthesia with halothane enhances
competitive blockade
D)
Competitive blockers do not cross
the blood-brain barrier
E)
Atracurium-induced blockade can be
reversed by acetylcholinesterase inhibitors
True/False Questions:
47. When a partial agonist is administered together with a full
agonist, the response will be less than that achieved compared to when the full
agonist is given alone.
48. Following peripheral administration of the two drugs,
neostigmine has better access to the brain compared to physostigmine.
49. For receptor binding of a ligand to a receptor measured in
the test tube, a linear plot of ligand bound on the y-axis vs. a linear plot of
ligand concentration on the x-axis produces a sigmoid (S-shaped) curve.
50. Drug A has a lower ED50 compared to Drug B for a specific
response. Therefore
Drug A has a greater potency compared to Drug B for this
response.
51. All G-protein coupled receptors produce their cellular
responses by altering cyclic AMP levels in the cell.
Mr. Mucho Regurgitation has recently had a successful mitral
valve
replacement operation for severe mitral regurgitation. His
echocardiogram 3 months after his open-heart surgery showed a good
functioning prosthetic mitral valve, but an enlarged left ventricle with
an ejection fraction of 35% and global hypokinesis. He does not complain
of any symptoms of heart failure, and is walking daily with a very good
functional status.
52.
Which of the following drugs would be expected to
have the SMALLEST or NO benefit on his long term survival?
A. Carvedilol
B. Enalapril
C. Digoxin
D. Lisinopril
E. Sustained Release Metoprolol
53. Which of the following statements regarding the cholinergic
system is correct?
A. Acetylcholine is the transmitter released by postganglionic
sympathetic neurons
B. The most important mechanism for removal of
acetylcholine from the synaptic cleft is enzymatic metabolism
C. Stimulation of the M2 muscarinic
receptor in the heart leads to increased myocardial contractility
D. Administration of methacholine
is likely to produce bronchodilation in a patient
with asthma
E. Only two muscarinic receptor
types (M1 and M2) are known to exist in humans
54. A 70 year-old man has slowing of
conduction in his atrioventricular (AV) node
resulting in a significant reduction in his ventricular rate and
hypotension. Given this information,
which of the following medications would be most appropriate for this patient?
A)
Acetylcholine
B)
Pyridostigmine
C)
Atropine
D)
Ipatropium
E)
Pilocarpine
55. Parasympathomimetic drugs are
categorized as either direct-acting or indirect-acting. Which of the following statements is
correct?
A)
Pilocarpine is an example of an indirect-acting parasympathomimetic drug
B)
A
direct-acting parasympathomimetic drug works by
directly blocking the muscarinic receptor on the
target organ
C)
An
indirect-acting parasympathomimetic drug works by
decreasing the breakdown of acetylcholine
D)
Donepezil (Aricept) is an example
of a direct-acting parasympathomimetic drug
E)
Both direct- and indirect-acting parasympathomimetic
drugs are approved for the treatment of gastrointestinal hypermotility
56. Which of the following statements
is correct regarding the autonomic nervous system?
A)
The
sympathetic nervous system arises primarily from craniosacral
outflow tracts
B)
The
division of the autonomic nervous system activated in response to emotional and
physical stress is called the parasympathetic nervous system
C)
The
primary catecholamine released by chromaffin cells in
the adrenal medulla is epinephrine
D)
Nicotine
is the neurotransmitter released by preganglionic
neurons
E)
The
neurotransmitter released by postganglionic parasympathetic neurons is norepinephrine
A 24 year old man arrives at the
emergency room after taking an overdose of amphetamines. His blood pressure is 180/100 and his heart
rate is 120.
57. What is the mechanism of
his hemodynamic changes?
A)
Direct
effects of amphetamine on alpha-1 and beta-1 receptors.
B)
Increased
stimulation of presynaptic alpha-2 receptors.
C)
Increased
release of norepinephrine into the synaptic cleft.
D)
Inhibition
of reuptake of norepinephrine from the synaptic
cleft.
A 70 year old man is being started
on terazosin for symptoms related to his benign prostatic hyperplasia.
He has no other medical diagnoses.
58. Which of the following adverse effects should you warn him about?
A)
Dizziness caused by low blood pressure
B)
Excessively
slowed heart rate caused by direct effects on the SA node
C)
Constipation
caused by relaxation of GI smooth muscle
D)
Shortness
of breath caused by bronchoconstriction
All available beta-adrenergic
antagonists block beta-1 receptors but their administration may result in
different therapeutic or adverse outcomes due to additional properties.
59. Which of the following is INCORRECT?
A)
Due
to its blockade of beta-2 receptors, propranolol
should not be administered to patients with asthma.
B)
Intrinsic
sympathomimetic activity (ISA) of pindolol
causes a relative increase in resting heart rate during sleep.
C)
Concurrent
blockade of alpha-2 receptors by carvedilol increases
the likelihood of hypotension with the drug.
D)
While
membrane-stabilizing activity is a characteristic of propranolol,
it is not apparent at therapeutic doses.
60. An 85 year old man with Alzheimer's
Disease is given donepezil. Which of the following should you anticipate
as an adverse effect of the drug?
A)
Constipation
B)
Urinary
incontinence
C)
Dry
eyes
D)
Sinus
tachycardia
61. Which of the following statements
is correct regarding the parasympathetic nervous system?
A)
Acetylcholine
is synthesized in the postganglionic neuron and is released passively into the
synaptic cleft.
B)
Activation
of presynaptic M1 receptors decreases release of
acetylcholine into the synaptic cleft.
C)
Removal
of acetylcholine from the synaptic cleft is primarily through reuptake and the process
is inhibited by cocaine.
D)
Stimulation
of M3 receptors in the heart result in decreased calcium permeability and
slowing of heart rate and AV nodal conduction.
62. A 6 year old child is seen in the
emergency room and has signs of severe organophosphate poisoning after
ingesting an unknown quantity of pesticide.
Which of the following statements is correct?
A)
Organophosphates
are classified as irreversible cholinesterase inhibitors.
B)
Atropine
improves symptoms in patients with organophosphate poisoning by increasing
production of acetycholinesterase.
C)
Respiratory
muscle fatigue and paralysis are effectively treated with high doses of
atropine.
D)
Due
to its toxicity profile, pralidoxime should be
withheld for the first 24 hours.
63. A 52 year-old male presents to your
office with complaints of exertional chest pressure, which occurs either with
physical activity or with emotional upset. You diagnose him with angina pectoris and initiate
treatment.
Therapy for angina may work by all of the following
mechanisms, except:
A)
reducing preload, thereby
decreasing wall stress, decreasing MVO2
B)
reducing heart rate, thereby
reducing MVO2
C)
reducing blood pressure, thereby
reducing wall stress, decreasing MVO2
D)
dilating coronary arterioles,
thereby increasing coronary blood flow
E)
increasing contractility, thereby
increasing coronary blood flow
64. For which of the following anti-anginal agents has a
secondary prevention benefit been demonstrated?
A)
Isosorbide dinitrate
B)
Sublingual nitroglycerin
C)
Metoprolol
D)
Amlodipine
E)
Diltiazem
65. The mechanism of action of ranolazine is:
A)
Reduces blood pressure and
therefore myocardial oxygen consumption
B)
Reduces both heart rate and blood
pressure and therefore reduced myocardial oxygen consumption
C)
Increases coronary blood flow
D)
Is unknown but may involve glucose
metabolism
66. As part of the patient’s treatment, anti-platelet therapy
is also administered. Which of the following agents interferes with the binding
of ADP to its platelet receptor?
A)
Abciximab
B)
Clopidogrel
C)
Aspirin
D)
Eptifibitide
Questions 67 - 71:
A 35 year old female presents to the hospital four weeks
after delivering her second child, with signs and symptoms of congestive heart
failure. Left ventricular ejection fraction is measured at 25% by bedside
echocardiography. Regarding her diagnosis of cardiomyopathy:
67. Ischemic cardiomyopathy and non-ischemic cardiomyopathy
have all of the following features in common, except:
A)
Decreased
left ventricular compliance
B)
Decreased
left ventricular systolic function
C)
Compensatory
left ventricular dilation
D)
Compensatory
increase in circulating catecholamines
E)
Diffuse
sub-epicardial left ventricular necrosis
68. In patients such as this, one is likely to find all of the
following, except:
A)
Pulsus
alternans
B)
Cardiomegaly
C)
Increased
LV end-diastolic pressure
D)
Coolness
of the extremities
E)
Pulsus
paradoxus
This patient is represented by the Pressure-Volume loop
shown above, labeled “Baseline”:
69. The pressure-volume loop labeled "Y"
might be generated by:
a. giving
volume
b. giving an
ACE-inhibitor
c.
giving a diuretic
d.
giving an inotropic agent
70. The patient may have gone from
the loop labeled “X” to her current “baseline” by:
A)
Giving volume
B)
Giving an inotropic drug
C)
Giving a diuretic
D)
Giving an ACE-inhibitor
E)
Giving
hydralazine
71. The distance “Z” may be increased by doing all of the
following, except:
A)
Increasing only contractility
B)
Increasing only afterload
C)
Increasing only preload
D)
Giving an ACE-inhibitor
PATHOLOGY QUESTIONS:
In the photo below, the fetal heart
has been rotated to the right.

Answer true (A) or false (B) for each
of the following questions about the structure marked with a white square. (1 point each)
72. In a normal fetus, it carries
well-oxygenated blood, a large portion of which enters the aortic arch and supplies
blood flow to the brain.
73. Postnatally,
in the presence of certain cardiovascular anomalies prostaglandin is given to
maintain patency.
74. In a normal fetus, the amount of
blood flow through this structure is only 25% as great as flow through the pulmonary
arteries.
Answer true (A) or false (B) for the
following statement: (1 point)
75. One of the features which differentiates the left ventricle from the right ventricle
is a smooth upper septal surface with no attached chordae
tendineae.
The lesion illustrated above was on
the extremity of an infant. Microscopically it showed aggregates of thin-walled
capillaries, closely packed and lined by endothelium. No capsule was
present.
76. Which of the following is a
correct statement regarding this lesion? (3
points)
A)
Though
this patient was an infant, this entity is most common in middle age
B)
This is the most
common vascular tumor and can present as a “strawberry type” in newborns
C)
The
lesion is always flat with no elevation
D)
These
lesions occur only in skin and mucous membranes
*************************************************************
Answer true (A) or false (B) for each of the following statements. (1 point each)
77. Dilated cardiomyopathy and myocarditis are entirely unrelated entities.
78. Myocardial disarray is a
microscopic feature of hypertrophic cardiomyopathy.
79. Among the causes of dilated
cardiomyopathy is chronic consumption of alcohol.
80. Lymphocytic
myocarditis is usually secondary to drug
hypersensitivity.
81. Which of the following vasculitides is not associated
with antineutrophil cytoplasmic
antibodies (ANCA)? (1 point)
A)
Polyarteritis nodosa
B)
Churg-Strauss syndrome
C)
Wegener granulomatosis
D)
Microscopic
polyangiitis
Match the region of the heart with
the coronary vessel supplying oxygenated blood to that region when the coronary
circulation is right dominant. (1 point each)
82. The anteroseptal
region
83. The posterior wall of the left
ventricle
84. The AV bundle and the posterior
aspect of the upper septum
85. The lateral wall of the left
ventricle
A)
Right
coronary artery
B)
Left
anterior descending coronary artery
C)
Left
circumflex coronary artery
D)
The
coronary sinus
86. The least likely association with mitral annular calcification is - (1
point)
A)
Calcification
of the aortic cusps
B)
Calcification
extending into the cardiac skeleton (central fibrous body)
C)
The presence of
a parathyroid tumor causing hypercalcemia
D)
Old
age
A random
Pathophysiology Question:
87. Which of the
following is not a determinant of myocardial oxygen demand (MVO2)?
a)
heart rate
b)
contractility
c)
preload
d)
hemoglobin content
e)
afterload
/
88. The above photo is of a mitral
valve. The pathology illustrated has developed over a period of: (1 point each)
A)
5-6
days
B)
5-6
months
C)
at
least several years
D)
the entire lifetime of a 70 year old person.
89. The initial event starting this
disease process was most likely:
A)
an
episode of diphtheritic myocarditis
B)
pharyngitis due to group A beta–hemolytic streptococci
C)
endocarditis due to Streptococcus viridans
90. During the acute phase of this
disease histopathology is least likely
to show:
A)
pancarditis
B)
bacterial
colonies in endocardial vegetations
C)
Aschoff bodies
D)
Anitchkow cells
91. The following question is related to
the photo above. In the photo the large dark nuclei are indicative of : (3
points)
A)
A
rhabdomyoma
B)
Glycogen
storage disease
C)
Myocyte
hypertrophy
D)
Premalignant dysplasia
E)
Mutation
of a myosin gene in a case of dilated cardiomyopathy
Fill in the blanks – 1 word each (1 point each)
92. There is an easily fragmented,
“benign” tumor which grows from the endocardium to
form a sessile or polypoid mass, usually in the left
atrium. It is the most common primary cardiac tumor in the adult. The name of
the tumor is _____________.
93.
_______ pericarditis often develops a few
days after onset of transmural myocardial infarction
and occasionally develops later as Dressler
syndrome. (Supply the adjective)
94. In one or two sentences describe a
clinical scenario which results in cardiac tamponade. (2 points)
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________