Questions 1 – 3:
A 45-year-old male presents to the hospital
12 hours after the onset of an anterior myocardial infarction. His initial
examination reveals findings consistent with congestive heart failure.
A Swan-Ganz catheter is placed and a Frank-Starling performance curve is
generated:
1. Administering a positive
inotropic agent (e.g. Digitalis) to this patient will:
-
Move the curve upwards and to the left
-
Move the curve downwards and to the right
-
Decrease the slope of the curve
-
Move the patient leftward along the same curve
-
Move the patient rightward along the same curve
2. If the patient is on the portion
of the curve in quadrant 3, he can be improved by moving him to the left
into quadrant This could be accomplished by giving a drug which:
-
Increases contractility
-
Decreases contractility
-
Increases preload
-
Decreases preload
-
Decreases afterload
3. In general, a patient would be described as being in cardiogenic
shock if they were in which quadrant:
-
Quadrant 1
-
Quadrant 2
-
Quadrant 3
-
Quadrant 4
A 50-year-old male presented to the hospital with a large inferior myocardial
infarction. Questions 4 – 12 refer to this patient:
4. On initial presentation to the hospital, the patient's pulse was
50 per minute (Normal pulse = 60 – 100 per minute). Pathophysiologic reasons
for this relatively slow pulse might have included all of the following,
except:
-
increased vagal tone associated with the inferior MI
-
third-degree A-V block with a junctional (A-V nodal) escape rhythm
-
sinus bradycardia due to SA (sino-atrial) node ischemia
-
second-degree A-V block with two-to-one A-V conduction
-
increased sympathetic tone associated with the inferior MI
5. On initial presentation to the hospital the patient's blood pressure
was low, with a reading of 90/60 mm Hg. Pathophysiologic reasons for his
low blood pressure might have included all of the following, except:
-
right ventricular infarction causing increased vascular resistance
-
right ventricular infarction causing low LV preload
-
hypovolemia (low intravascular volume)
-
reduced vascular resistance from increased vagal tone
-
reduced cardiac output related to the MI
6. The pathophysiology of his acute myocardial infarction might have
involved all of the following, except:
-
a "wavefront" spread of ischemia and infarction from the endocardium
to the epicardium
-
plaque rupture with platelet aggregation and thrombosis
-
release of serum catecholamines exacerbating ischemia
-
increase in left ventricular wall tension
-
increase in left ventricular compliance
7. All of the following are determinants of this patient's myocardial
oxygen supply, except:
-
viscous coronary resistance
-
compressive coronary resistance
-
hemoglobin content
-
wall tension
-
cardiac output
On day four of the hospitalization, the patient develops a new systolic
heart murmur and the following oxygen saturations and pressure curves are
obtained with a Swan-Ganz catheter:
|
Oxygen Saturation
|
Pressure (mm Hg)
|
|
Right Atrium
|
62%
|
8
|
|
Right Ventricle
|
61%
|
30/8
|
|
Pulmonary Artery
|
61%
|
30/22
|
|
Pulmonary Capillary Wedge
|
60%
|
22 mean
V-waves to 50
|
8. This patient's echocardiogram might be
expected to show:
-
Acute ventricular septal defect
-
Acute mitral regurgitation
-
Acute left ventricular free wall rupture
-
Acute right ventricular infarction
-
Acute left ventricular apical aneurysm formation
9. An intra-aortic balloon pump placed in this
patient might improve his hemodynamics by:
-
Decreasing left ventricular afterload during
systole
-
Increasing left ventricular afterload during
systole
-
Decreasing left ventricular preload during diastole
-
Increasing left ventricular preload during diastole
10. The likely gross pathologic finding in the
affected portion of this patient's heart muscle is:
-
White, fibrotic thinned myocardium
-
Red, hemorrhagic thickened myocardium
-
Normal appearing myocardium
-
Purple, discolored firm myocardium
-
Yellow, softened myocardium
This patient's pulmonary capillary wedge pressure
tracing is seen below.
-
What is the correct title for the section labeled
1?
-
Pulmonary capillary wedge pressure
-
The dicrotic notch
-
The A-wave
-
A small V-wave
-
A giant V-wave
12. What is the correct title for the section labeled 2?
-
Pulmonary capillary wedge pressure
-
The dicrotic notch
-
The A-wave
-
A small V-wave
-
A giant V-wave
Questions 13 – 16:
A 60-year-old male patient presents with a
history of palpitations, shortness of breath on exertion, and fatigue.
The patient indicates that his palpitations are felt as irregular heartbeats,
occasionally rapid, and sometimes associated with lightheadedness. An electrocardiogram
is obtained and lead II is shown below:
-
The electrocardiogram shows:
-
a chaotic atrial rhythm without discrete P waves
-
deep "sawtooth" flutter waves
-
advanced heart block
-
ventricular fibrillation
14. This patient's arrhythmia has been shown
to :
-
be present in up to 5% of adults over 65 years
of age
-
never occur in patients with pneumonia
-
predominantly occur in children
-
rarely require hospital admission for evaluation
and treatment
15. The patient is worried about the possible
complications associated with his arrhythmia. Warfarin (coumadin) might
be indicated to:
-
prevent ventricular tachycardia
-
reduce the risk of bleeding complications
-
correct thyroid function abnormalities
-
anticoagulate the patient and prevent embolic
strokes
16. The patient is treated with quinidine, and
following only a few doses, you are informed that he has had syncope and
that the electrocardiogram shows "twisting of the points". You conclude
that:
-
the patient has Wolff-Parkinson-White syndrome
-
the patient has developed "Torsades de pointes",
as a pro arrhythmic complication of quinidine
-
the patient has probably not been taking his
quinidine
-
the patient is having an acute myocardial infarction
A 38 year old Hispanic woman presents to the
Emergency Room complaining of marked shortness of breath which began suddenly
about two hours ago. On exam, her heart rate is 140 beats per minute. Cardiac
auscultation is difficult because of her rapid heart rate. She has moist
rales over both lung fields. Her chest X-ray shows pulmonary edema with
elevation of the left mainstem bronchus, a double density and straightening
of the left heart border.
-
What two diagnostic tests would be most helpful
to further evaluate this patient?
-
transthoracic echocardiography and an electrocardiogram
-
cardiac catheterization and cardiac MRI
-
phonocardiography and transesophageal echocardiography
-
radioisotope nuclear stress testing and cardiac
MRI
-
transthoracic echo and transesophageal echo
18. What is her most likely valve lesion?
-
Aortic stenosis
-
Aortic insufficiency
-
Mitral stenosis
-
Mitral insufficiency
-
Tricuspid insufficiency
19. Why did she develop pulmonary edema?
-
increased left ventricular preload
-
increased left ventricular afterload
-
decreased left ventricular systolic function
-
increased left atrial pressure
-
pulmonary embolic disease
20. All of these next choices can be used to
help treat this patient, except:
-
medication to slow the heart rate and increase
diastolic filling time
-
diuretics to lower pulmonary capillary wedge
pressure
-
cardioversion, if the heart rhythm is atrial
fibrillation
-
anticoagulants to prevent left atrial thrombus
formation
-
medication to lower left ventricular afterload
Questions 21 – 23:
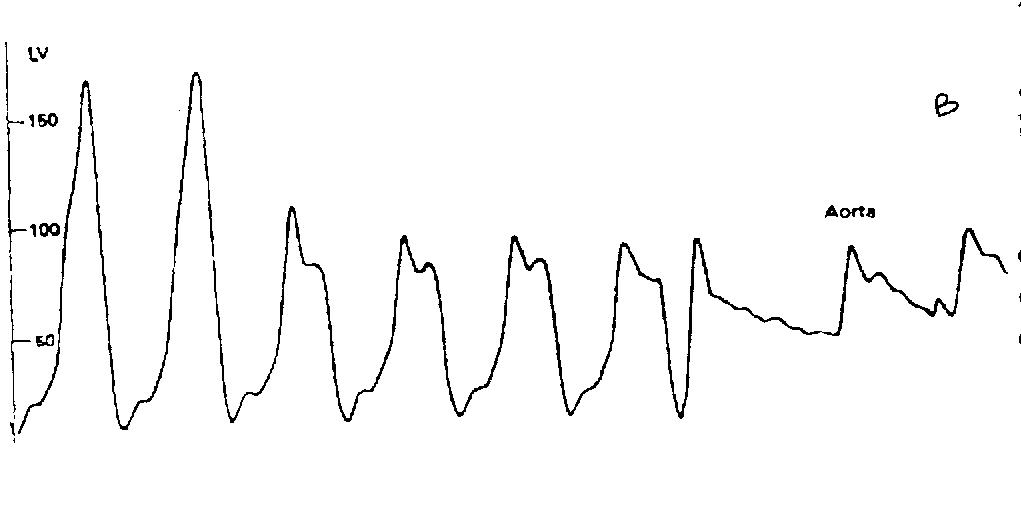
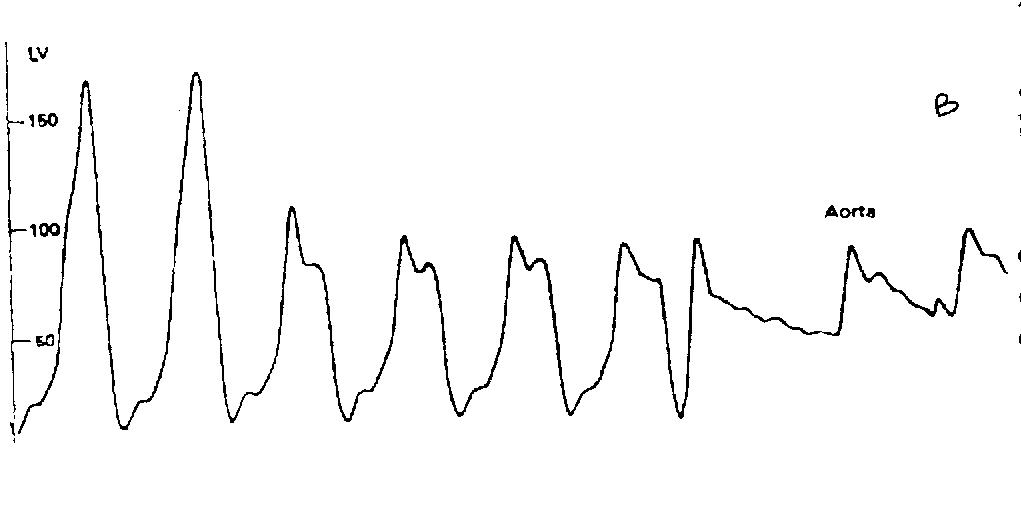
Withdrawal pressure tracing from the
left ventricle to the aorta
A 25-year-old male with a diagnosis of cardiomyopathy
experienced dizziness while playing basketball. Examination revealed a
blood pressure of 130/85 mm. Hg; regular pulse at 85/minute, and normal
respirations. He had no jugular venous pressure elevation, his lungs were
clear, and cardiac examination revealed a forceful apical impulse, normal
S1 and S2; an S4 was present as well as a grade 3/6 systolic murmur between
the apex and left lower sternal border.
21. Based on the left ventricular to aortic
pullback pressure tracing shown in the figure above, what advice would
you give this patient regarding participation in sports?
-
Avoid all sports
-
Avoid prolonged aerobic sports
-
Avoid contact sports
-
Avoid table tennis
22. Medical management should aim at (choose
one):
-
reducing preload
-
decreasing contractility
-
increasing contractility
-
reducing afterload
23. What effect would the Valsalva maneuver have
on the murmur?
-
Murmur intensity would be accentuated.
-
Murmur intensity would be diminished
-
No change.
Questions 24 – 25:
Electrocardiogram (top tracing)
IN = inspiration
EX = expiration
Arterial Blood
Pressure (bottom tracing)
A 45-year-old male with history of metastatic
disease from bronchogenic carcinoma was admitted with hypotension and diaphoresis.
His arterial pressure tracing is shown in the figure.
-
What is the two-word term for this pathophysiologic
phenomenon?
(Please write into the answer sheet)
-
What condition does this patient have?
-
Dilated cardiomyopathy
-
Acute right ventricular infarction
-
Hypertrophic cardiomyopathy
-
Constrictive pericarditis
-
Cardiac tamponade
26. "Kussmaul's sign" is most prominent in which
one of the following conditions?
-
Dilated cardiomyopathy
-
Acute ventricular septal defect
-
Hypertrophic cardiomyopathy
-
Constrictive pericarditis
-
Cardiac tamponade
27. What is the pathophysiologic mechanism of
Kussmaul's sign?
-
During inspiration, right ventricular filling
is augmented, and left ventricular filling falls, thereby lowering blood
pressure
-
During expiration, right ventricular filling
is augmented, and jugular venous pressure rises
-
During inspiration, negative intrathoracic pressure
is not transmitted to the right atrium and right ventricle, and jugular
venous pressure rises
-
During expiration, positive intrathoracic pressure
is not transmitted to the right ventricle, and the intraventricular septum
bulges to the right, causing jugular venous pressure to rise
Questions 28 - 29:
A 30-year-old woman develops progressive shortness
of breath and fatigue two months after delivery of a child. Blood pressure
is 140/90 and her pulse is 60/minute. She has jugular venous pressure elevation,
minimal rales bilaterally and a third heart sound (S3). She has mild pitting
edema of her legs. Her cardiac size on chest x-ray is mildly enlarged.
An echocardiogram shows no structural defects but the left ventricular
ejection fraction is 30%.
28. The most likely diagnosis is:
-
Hypertrophic cardiomyopathy
-
Dilated cardiomyopathy
-
Restrictive cardiomyopathy
-
Congenital V.S.D.
29. The most appropriate treatment combination
is:
-
Diuretics and an angiotensin converting enzyme
inhibitor
-
Nitrates and diuretics
-
Digoxin and diuretics
-
Beta-blocker and diuretics
-
Beta-blocker and calcium-channel blocker
* * * * * * * * * * * * * * * * * *
30. The compliance of the left ventricle can
be defined by relating change in pressure to change in volume during left
ventricular filling. This LV compliance is defined as:
-
 V/
V/  P
P
-
 P/
P/  V
V
-
 P x
P x  V
V
-
 P x
P x  V / 2h
V / 2h
-
P x r / 2h
(where  V = change in volume,
V = change in volume,  P =
change in pressure, h = wall thickness, and r = LV radius)
P =
change in pressure, h = wall thickness, and r = LV radius)
Questions 31 – 36 have True or False answers
(1/2 point each):
There are three shunt pathways that are instrumental
in the fetal circulation.
-
One of these pathways is called truncus arteriosus
-
One of these pathways is called ductus venosus
-
One of these pathways is called the interventricular
foramen
-
One of these pathways is called the foramen ovale
-
One of these pathways is called septum primum
-
One of these pathways is called ductus arteriosus
- - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - -
-
A one-year-old boy has a congenital ventricular
septal defect. Which of the following is not a determinant
of the amount and direction of shunted blood flow through the abnormal
communication?
-
The size of the defect
-
The location of the defect
-
The pulmonary vascular resistance
-
The aortic (systemic) vascular resistance
- - - - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - -
Questions 38 – 40:
A 72-year-old male with long-standing hypertension
has an echocardiogram, which demonstrates concentric left ventricular hypertrophy
with normal systolic function, and impaired diastolic filling. His electrocardiogram
shows normal sinus rhythm.
38. This patient's "compensatory" left ventricular
hypertrophy:
-
Increases wall tension (wall stress)
-
Decreases wall tension
-
Increases afterload
-
Increases preload
-
Decreases myocardial oxygen demand
39. If this patient's rhythm changed to atrial
fibrillation, there would be loss of the "atrial kick", which might cause
a 10 – 30% fall in cardiac output. This "atrial kick" occurs:
-
Immediately before opening of the mitral valve
-
Immediately after opening of the mitral valve
-
Immediately before closure of the mitral valve
-
Immediately after closure of the mitral valve
-
This patient's myocardial oxygen demand might
be increased because of:
-
Decreased contractility from left ventricular
hypertrophy
-
Increased contractility from left ventricular
hypertrophy
-
Decreased wall tension from left ventricular
hypertrophy
-
Increased wall tension from left ventricular
hypertrophy
* * * * * * * * * * * * * * * * * * *
* *
Questions 41 - 43:
You are asked to see three patients in consultation.
Each has been told that he/she has valvular heart disease as determined
by a catheterization performed at a distant hospital. Each patient was
given a copy of his or her catheterization report. Based on the information
provided, what primary valvular abnormality best explains the findings
for each patient?
|
Patient A |
Patient B |
Patient C |
| Aortic Pressure |
160/50 |
120/80 |
110/90 |
| LV Pressure |
160/10 |
120/6 |
200/18 |
| PCW Pressure |
a=6,v=10
mean=8 |
a=25,v=22
mean=20 |
a=18, v=22
mean = 18 |
| PA Pressure |
25/12 |
75/35 |
40/15 |
| RV Pressure |
25/5 |
75/15 |
40/8 |
| RA Pressure |
a=4,v=4
mean=4 |
a=15, v=25
mean=18 |
a= 5, v=6
mean = 5 |
| Murmur(s) |
Diastolic |
Diastolic and systolic |
Systolic |
| LV ejection fraction |
85% |
55% |
60% |
(where LV = left ventricle, PCW = pulmonary
capillary wedge, PA = pulmonary artery,
RV = right ventricle, RA = right atrium)
-
Patient A has:
-
Aortic stenosis
-
Aortic insufficiency
-
Mitral stenosis (primary) and tricuspid regurgitation
(secondary)
-
Acute mitral insufficiency
-
Chronic mitral insufficiency
42. Patient B has:
-
Aortic stenosis
-
Aortic insufficiency
-
Mitral stenosis (primary) and tricuspid regurgitation
(secondary)
-
Acute mitral insufficiency
-
Chronic mitral insufficiency
43. Patient C has:
-
Aortic stenosis
-
Aortic insufficiency
-
Mitral stenosis (primary) and tricuspid regurgitation
(secondary)
-
Acute mitral insufficiency
-
Chronic mitral insufficiency
* * * * * * * * * * * * * * * * * * *
* * * * * * *
Workspace area
This diagram of normal pressures is included to help you work through
Questions 41 – 43.
BONUS QUESTION
44. In the above flow-volume loop,
the patient might be moved from curve 3 to curve 1 by:
-
Administering a diuretic
-
Administering an inotropic agent
-
Administering a venous dilator
-
Administering an arterial vasodilator
-
Decreasing left ventricular contractility