Link strengthens between mitochondria and synapses in autism
A recent study bolsters the link between autism and mitochondrial dysfunction. After looking at gene expression patterns from dozens of post-mortem brains, Carney Institute researchers found reduced activity of mitochondrial genes in the brains of individuals with autism.

“It’s unclear what causes the clinical syndromes that we recognize as autism,” said Matthew Schwede MD’15, lead author of the study. “But despite the condition’s heterogeneity, we were able to find links that were present across many individuals with autism.” Mitochondria are structures that generate energy within cells. Mounting evidence over the past few decades suggests that mitochondrial abnormalities are associated with autism, as well as with schizophrenia and bipolar disorder. The team re-analyzed gene expression data from the four largest published studies that compared the cerebral cortex of brains donated by individuals with autism and by individuals without autism. Called transcriptome analysis, this technique allows researchers to understand which genes are being expressed.
The study, published last month in the Journal of Neurodevelopmental Disorders, found that genes related to mitochondrial function show decreased gene expression in autism cerebral cortex. This means that these genes had lower levels of messenger RNA, a type of genetic information based on DNA that gives directions for protein creation. The researchers believe that this decreased expression is a result of downregulation, or a decrease in expression due to gene regulation.
Previous studies using these datasets have found that genes related to synapse function in the cerebral cortex of individuals with autism are also downregulated, which Schwede’s study corroborated. The levels of expression of genes related to synapse function and mitochondrial function are strongly correlated. “The overarching result from the analyses is that in the autism brain, there seems to be a signature of an abnormality in mitochondrial function that’s tightly linked to an abnormality in synapse function,” said Eric Morrow, co-director of the Center for Cells and Circuits within the Carney Institute, and senior author of the study. “So mitochondrial function at the synapses may be altered in autism.”
While it’s unclear what that link is, the correlation between these genes suggests that the two functions are co-regulated, Schwede said. “A single factor could cause downregulation of both synapse-related genes and mitochondria-related genes, or one process could be leading to the other,” Schwede said. “When synapses aren’t in use as much, a cell doesn’t need as much energy, so it could downregulate mitochondria. Or vice versa. If mitochondria were downregulated, you could imagine that synapses wouldn’t be as functional, and thus the synapse-related genes would also get downregulated.”
Mitochondrial abnormalities have been implicated in other psychiatric conditions, according to another study published in February that shares two authors with Schwede’s paper. The February study also used transcriptome analysis and showed that schizophrenia and bipolar disorder are associated with downregulation of mitochondria- and synapse-related genes. Furthermore, Schwede’s study provides evidence for another common link between autism and schizophrenia. In previous studies of autism and schizophrenia, researchers have found abnormalities in brain cells called cortical inhibitory interneurons. These cells help regulate the balance between excitatory and inhibitory signals in the brain. Schwede’s analysis showed that one of the most strongly downregulated genes in the brains of individuals with autism was associated with inhibitory interneurons.
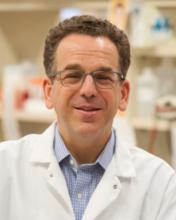
“It’s hard to know exactly what these overlapping transcriptome signatures mean at this point, except seemingly different disorders appear to share some aspects of the underlying biology,” Morrow said. While the clinical presentations of conditions like autism and schizophrenia may be different, “the causes of circuit failure or the way those circuits fail may have some similarities,” he added. However, transcriptome analyses cannot be used to determine cause or effect, so it’s unclear whether these downregulated genes lead to autism or if autism causes these abnormalities. Morrow’s lab, which currently focuses on the role that mitochondrial biology plays in learning disorders, is working to figure out the answer. “We’ve taken a number of the genes that we have found to be misregulated and we’re making mutations in them to see whether primary changes in them can lead to pathology that is autism-like,” Morrow said. This research is conducted using experimental systems such as mouse models and human stem cell lines.
Future research could also examine whether treatments targeting mitochondrial function are useful in reducing the symptoms of autism, Schwede said. The study highlights two essential components of human neuroscientific research: the ability to look at the human brain in postmortem studies and the broad sharing of data. These tissues are so important to the field that national efforts, such as the Autism BrainNet, are working to develop a shared brain bank for such autism studies, said Morrow, a founding member of the Scientific Review Committee at Autism BrainNet. Data sharing further helps maximize families’ and funders’ contributions to research.
The research was funded by the Burroughs Wellcome Fund, National Institutes of Health, Simons Foundation Autism Research Initiative and Hassenfeld Child Health Innovation Institute at Brown University.
Other authors include Shailendar Nagpal, former bioinformatics specialist at Brown University; Michael J. Gandal and Daniel H. Geschwind from the University of California at Los Angeles; Neelroop A. Parikshak, formerly from UCLA; and Karoly Mirnics, formerly from Vanderbilt University.



