Guest Column: Is the opioid epidemic a global phenomenon?
“Tootan” (breaking) is the Hindi-Urdu word for drug withdrawals. In ethnographic work with heroin addicts in north India, I repeatedly encountered this word in moving accounts by treatment-seekers, caregivers and family members as they described the screams and agony, the “tootan,” the increasing intensity of which might be a tipping point for treatment seeking or the prelude to an opioid-related overdose death.
Opioids were not initially part of my research design on urban poverty and mental health in India that I began in 2015. As I started to notice the magnitude and ubiquity of opioid-related addiction issues in my field sites in lower-income neighborhoods in Delhi, and then back here in the U.S., I began to wonder what a comparative, global picture of the opioid epidemic might look like. As a Carney Institute fellow, I hope to create a research consortium on the theme of global opioids.
My host institutions for this research in India, the All India Institute of Medical Sciences (AIIMS) Psychiatry and the National Drug Dependence Treatment Centre (NDDTC), were overseeing the largest national survey of opioid use and abuse in India so far, published in 2019. With a small research team, I began to piece together available figures and secondary literature from across the world, with the question in mind: is the opioid epidemic a global phenomenon? The brief answer is yes, but with critical variations, at times within nations, and across western and non-western contexts. Consider India as a case in point.
The situation in India
As with most efforts at comparative quantification, data for developing world countries is harder to come by and often less “reliable” than in western contexts. For instance, in India, precise numbers of overdose deaths are much harder to quantify because deaths, particularly among the homeless, are often registered in mortuary records as “cause unknown,” or with entries such as “death by exposure to cold” or heat, depending on the season.
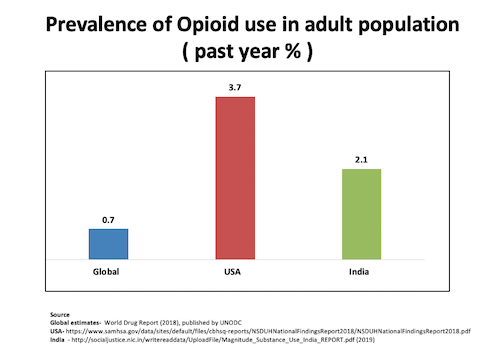
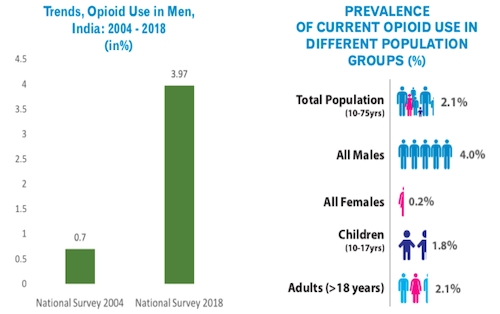
Uncertainties notwithstanding, there have been two major national surveys of opioid use and abuse in India, in 2004 and 2019, conducted by AIIMS Psychiatry and the National Drug Dependence Treatment Centre. The most recent survey found that the prevalence of opioid use in India is three times the global average. About 2.1% of India’s population use opioids. India still has lower figures than the United States for opioid use prevalence, but this may change in years to come, as pharmaceutical companies begin to more aggressively target developing world markets, and obliging right wing governments—such as the one currently in power in India—gradually widen the range of available opioids.
India’s previously stringent Narcotic Drugs and Psychotropic Substances Act was amended in 2014 to create a new class of medicines called “essential narcotics,” including fentanyl, oxycodone, codeine and hydrocodone. Many of the stars of the American opioid epidemic are gradually becoming more widely available in India.
My own ethnographic fieldwork has been based in opioid substitution treatment programs in urban poor neighborhoods in Delhi. Building on this research and the uncertain process of overhearing conversations in other disciplines, I will point to two potential domains of further research in engaging with the sharply varying and yet global nature of the opioid epidemic. The first domain calls for collaborations across anthropology, social psychiatry, and public health, while the second traverses somewhat uncharted territory with possibilities for collaboration between anthropology, philosophy and neuroscience, in thinking about questions of pain and vitality.
Understanding variations within seemingly similar contexts
To say that a phenomenon is global is not to say that it is uniform. I first began to think about the significance of local variations in the course of fieldwork as I encountered a striking difference between two proximate and demographically and economically similar urban poor “resettlement” neighborhoods in Delhi: Trilokpuri and Sunder Nagri, where AIIMS Psychiatry runs Opioid Substitution Therapy (OST) clinics.
As most heroin addicts describe it, in India and elsewhere, there are three ways to ingest heroin. You can smoke it, which is relatively expensive, costing roughly Rs. 250 ($3.50) a piece in Delhi. You can chase it, on a foil, which is slightly cheaper, about Rs. 200 ($2.80). And after that, come the “injectors” with sui (injections) and sheeshi (bottles with opioid pharmaceutical cocktails), easily available illegally in India, which one buys at chemist shops and not from a drug dealer for Rs. 40 ($0.50) or less—one fifth the price of a smoker or chaser’s habit. As most addicts put it, “a chaser’s life is ten years long; an injector’s life is two years at most.” Addiction psychiatrists would agree, pointing to various vulnerabilities for injectors including the risk of contracting HIV or Hepatitis B through shared needles.
Staying in both these neighborhoods in Delhi for extended periods of time, conducting repeat interviews with patients and caregivers over the last three years, studying patient files, and conducting household surveys in both neighborhoods, a sharp difference in the mode of consumption gradually began to emerge more clearly: the neighborhood of Trilokpuri had barely a single injector (and I say this after visiting every drug dealer, and every spot in and around the neighborhood where addicts hang out). In contrast, in the neighborhood of Sunder Nagri, used injections could be found everywhere, strewn in ordinary neighborhood spaces such as parks.
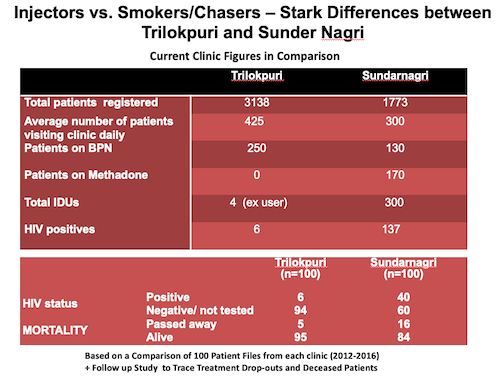
Numerically, the difference is quite stark. According to current clinic figures, out of 3,138 patients in Trilokpuri, there are only four injecting drug users (IDUs) and six HIV+ patients. In contrast, in Sunder Nagri out of a total of 1,773 patients, 300 are IDUs and 137 are HIV+. On a national scale, IDUs in India show a much higher rate of HIV than for instance commercial sex workers, often assumed to be the primary drivers for the spread of HIV. These seemingly “local” differences can be a question of life and death, in better understanding the ways in which the epidemic plays out in particular geographies.
What causes such differences between otherwise similar local ecologies? I am in the process of writing a research article on this comparison of Delhi neighborhoods, but the question extends much beyond Delhi. These ecological differences are equally important in other parts of the world, including in the United States, where more recent opioid related research tracks neighborhood level variation, rural-urban differences, as well as significant regional differences between the American South, northeast and Midwest in patterns of opioid abuse and mortality rates even between demographically similar areas. As many scholars in this current wave of research have argued, understanding such variations can have significant consequences for the ways in which treatment and intervention might be imagined.
Heroes and Heroin: Somewhere between vitality and pain
A second domain of potential interdisciplinary conversation is around seemingly subjective experiences such as pain, as differently approached, for instance, in anthropology and in ongoing work in neuroscience at Brown University. In what ways might we connect different units of analysis, the neuronal, the social, and the global, while retaining the specific complexity of these different “ecologies of mind,” rather than making it solely a question of “scale?” One way to do this in the case of opioids might be to unsettle one of the key assumptions in the scholarly literature on this issue, namely that the opioid epidemic is only about pain.
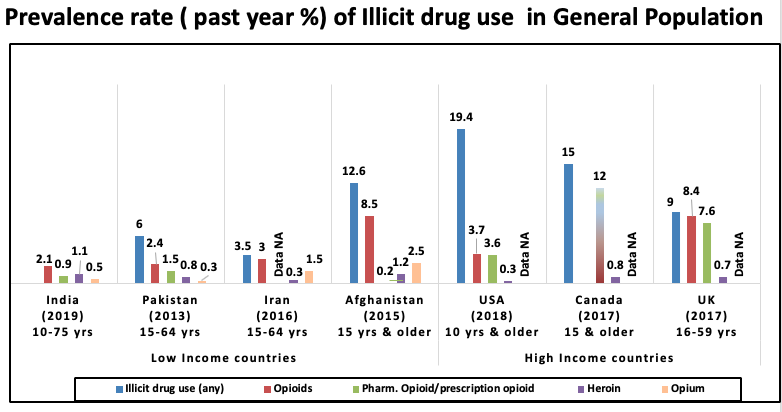
Consider, for a moment, a sharply global difference, namely, the quite distinct mode of opioid consumption and contagion between western and developing contexts. In western contexts the opioid epidemic is primarily driven by prescription-opioids. In contrast, in non-western contexts, rather than being physician driven, or a symptom of prescription opioid overconsumption, at least at present, the epidemic is more directly a form of heroin addiction. Even for people who inject drugs in non-western contexts, the opioid infused pharmaceutical cocktails they inject are a continuation of heroin–related addiction trajectories that are not prescription driven. Qualitatively, what kind of a difference is this?
In understanding this difference, readers from the “harder” sciences might need to make a leap of faith into the anthropological engagement with affects and emotions, and the not always “anecdotal” evidence that we offer, in asking you to join us in this leap or step. Conceptually, let us ask: what is the experience of heroin? What kind of a “trip” is it, if it is not primarily hallucinogenic?
I first began to think about this question in the course of my ethnography of OST clinics in India. Heroin addicted patients in urban poor neighborhoods in Delhi (and across India) are overwhelmingly male. In contrast, caregivers (and, as it happens, drug dealers in north India) are mostly female. Male patient addicts often exuded a kind of self-destructive volatility that I sensed but didn’t quite know how to name it, a quality of life and energy that made terms like chronic pain, abjection, alienation, and numbness somehow feel inadequate.
How might we conceptualize this form of volatility? A footnote in the history of heroin that I chanced upon opened up a new conceptual possibility. How did heroin come to be named as such? In 1895, Felix Hoffmann, a German chemist working at Bayer Pharma, still one of the leading pharmaceutical companies in the world, resynthesized diamorphine in an attempt to produce a less addictive opiate. The experiment mistakenly produced a substance twice as powerful as morphine, which, for the next 12 years or so, was assumed to be non-addictive. This being the era before ethics approvals, Hoffmann initially tried out the new substance on factory workers at the Bayer head office in Germany, who reported that it made them feel “heroisch” (heroic).
The word hero comes from the Greek word heroon, a shrine meant to commemorate a kind of ambivalent, potentially harmful potency. In light of this energetic valence, I suddenly saw my addict interlocutors more clearly: pickpockets, younger initiates and retired toughs with their jail records and colorful pet names. I was among fallen or falling “heroes,” who in the case of India happen to be male, but those who have spent time with addicts, even in other parts of the world, will know the swagger or quality I invoke, which may be expressed regardless of gender. We might view the “heroic” dimension of heroin not entirely as a delusion, but rather as a potentially botched experiment with vitality.
What are the forms of life and death that emerge around these experiments with vitality? Anthropologically, I began to understand a social dimension of heroin (as it spread in different waves or “epidemics” of consumption, as these emerged in urban poor neighborhoods in Delhi) as part of a kind of “rite of passage,” as the canonical social theorist Arnold van Gennep called it. Reconceived as such, I began to better understand the narratives of addicts and their turn to heroin (called “smack” in India), with its promise of an increase in sexual potency and extended time to ejaculation, and addiction trajectories in relation to the Hindi-Urdu term josh (energy) needed for initiation into gang cultures and unorthodox livelihoods such as pickpocketing, the occupation most commonly listed in clinical files as a heroin addict’s calling in north India.
With this speculative and empirical invocation of vitality, we seem to have strayed quite far from the sciences. Or maybe not? The Bergson-influenced psychiatrist Eugene Minkowski had offered a conception of vitalism (or the “loss of vital contact with reality”) as key to understanding a variety of mental illnesses. Could an anthropologist engage with a neuroscientist, for instance, on as ephemeral a concept as vitality?
My own very tentative, layperson’s initiation into neuroscience came through a friend and interlocutor, now deceased, Catherine (Cathy) Kerr, one of the co-founders of the Contemplative Studies Program at Brown. With Cathy, I first began to co-teach and think about how we might use conceptual categories from non-western traditions of thought, focused on notions of vitality, such as prana and qi, however difficult and uncertain the synaptic transmission may be between ontologies, geographies and disciplines across the arts and sciences.
Inspired by these conversations with Cathy, I wrote an article on the idea of vitality as a concept for anthropological thought. In Fall 2020 a group of neuroscientists at Brown will be organizing a Kerr Energy conference. In anticipation of these as yet uncharted territories, I wish to dedicate this piece to Cathy, in honor of her exemplary traversal across geographies, times, disciplines and otherwise disparate branches of knowledge, in the hope of continuing our own sometimes botched adventures with scholarly vitality, which might continue even across the uncertain thresholds of life and death. The opioid epidemic is global, and getting worse. That said, the geographic and psychic variations that I suggest above might be crucial in understanding some of the threats and possibilities, and as yet unknown ways forward.
Bhrigupati Singh is an assistant professor of anthropology at Brown University. From academic year 2020-21, he will serve as associate professor of anthropology and sociology at Ashoka University in India, visiting associate professor of psychiatry at Brown University, and a research fellow at the Carney Institute for Brain Science, co-organizing a research consortium on global opioids.



