The medical and mental health fields use standard terms and criteria for diagnosis for mental health disorders derived from the DSM-IV-TR (APA, 2000). It is important for justice staff to familiarize themselves with the mental health disorders that most often co-occur with alcohol and other drug problems. The following descriptions are drawn from CSAT’s TIP 42: Substance Abuse Treatment for Persons with Co-Occurring Disorders (CSAT, 2005b).
Personality Disorders
These individuals often have personality traits that are persistent and cause impairment in social or occupational functioning and personal distress. Symptoms are evident in their thoughts (ways of looking at the world, thinking about self or others), emotions (appropriateness, intensity, and range), interpersonal functioning (relationships and interpersonal skills), and impulse control.
An example of a personality disorder is Borderline Personality Disorder. These individuals typically experience many specific negative emotions like vulnerability, hostility, sadness, and anxiety or a nonspecific but intense sense of distress or “feeling bad.” This is combined with an inability to monitor and control emotions, alternating chaotic or contradictory ways of relating to self and others, and self-harming or dramatically self-destructive behaviors.
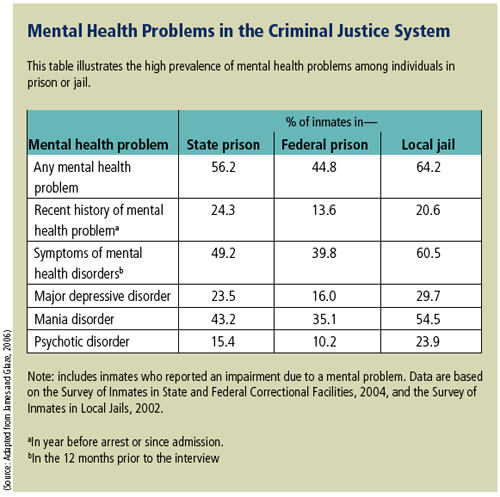
Psychotic Disorders
The common characteristics of these disorders are symptoms that focus on problems of thinking. The most prominent (and problematic) symptoms are delusions or hallucinations. Delusions are false beliefs that significantly hinder a person’s ability to function. For example, an individual may believe that people are trying to hurt him/her. Hallucinations are false perceptions in which a person sees, hears, feels, or smells things that are not real (i.e., visual, auditory, tactile, or olfactory).
Psychotic disorders are seen most frequently in mental health settings and, when combined with substance use disorders, the substance disorder tends to be severe. Drugs like cocaine, methamphetamine, or phencyclidine can produce delusions and/or hallucinations as well as drug intoxication.
Mood Disorders
Depression, mania, bipolar disorder, anxiety, and post-traumatic stress disorder are examples of mood disorders. Generally, an individual with a mood disorder experiences feelings or emotions to the extreme. Many people with substance use disorders also have a mood disorder and tend to use a variety of drugs.
There is a high prevalence of Post-traumatic Stress Disorder (PTSD) in the justice system. One study found 34% of female jail inmates had PTSD (Teplin et al., 1996). Problematic early life experiences, physical and sexual abuse, witnessing violence among family and friends, and other traumatic life events often emerge as key issues in substance abuse treatment. Whether identified initially or during treatment, it is important that these issues are addressed as soon as possible and incorporated into the treatment plan. While most individuals will find that their negative mood will decrease over the first few months of abstinence and treatment, their depression, nightmares, and other trauma-related symptoms might persist several months. If symptoms are not severe enough to require treatment at a mental health services program, the individual should be referred to mental health professionals for further assessment and treatment. They could be recommended for antidepressants and/or anti-anxiety medications with cognitive-behavioral therapy. These interventions may be instrumental in keeping an individual engaged in treatment and less likely to relapse.
Trauma and Abuse
Research shows that rates of trauma in men and women entering the justice system are higher than rates found in the general population. A history of physical and/or sexual abuse has been linked to many types of mental disorders, including PTSD, depression, suicidal behavior, borderline personality disorder, and other personality disorders (Spielvogel and Floyd, 1997).
Psychopathy
Psychopathy is a criminogenic risk factor often found among offenders with substance use disorders. Psychopathy is marked by primary and severe deficits in attachment and interpersonal bonding, lack of empathy for others’ experiences, lack of remorse, and shallow emotional functioning. Ten to 20% of male prison inmates meet the criteria for psychopathy (Hare et al., 1991).









