
Research on the biology of substance use disorders can help explain why these problems persist despite their negative impact on the health and safety of individuals, families, and communities.
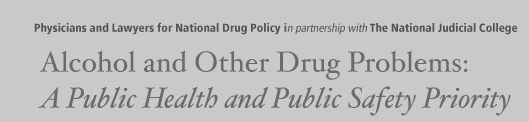
What determines if an individual will become addicted or not? Developing substance use disorders is a function of a number of interacting factors related to the individual, such as genetics and gender; the type of drug, the amount taken and method of delivery; and the environment in which the substance is used. These factors can both decrease or increase the risk that an individual will develop a problem. Factors that increase the risk are called risk factors; factors that decrease the risk are referred to as protective factors (McLellan et al., 2000; O’Brien, 2003).
Research shows that genetic factors account for between 40% and 60% of an individual’s vulnerability to developing substance abuse problems, including the effects of environment on gene expression and function. Environmental factors that influence an individual’s vulnerability to developing problems include home, family, school, and peers. Adolescents and individuals with mental health disorders are at greater risk of developing alcohol and other drug disorders than the general population (NIDA, 2007). Another factor that is important to consider is the age of first use of substances. Compelling data demonstrate that the younger a person is at the onset of substance use, the more likely they are to develop a substance use disorder and to continue that disorder throughout adulthood. In 2006, adults aged 21 or older who first used alcohol before age 21 were more likely (9.6% vs 2.4%) than adults who had their first drink at age 21 or older to be classified with alcohol or drug dependence or abuse (SAMHSA, 2007). Recent research by Drs. King and Chassin (2007) found that early (age of 13 or younger) drug use triples the odds of an adolescent developing drug dependence in adulthood. However, early alcohol and other drug use does not always result in later abuse and dependence; but it is a risk factor that may increase the likelihood of developing a problem (King and Chassin, 2007).
Why do people use People may use alcohol and other drugs for many reasons including relief of withdrawal, particularly in the criminal justice settings. To feel good Most drugs, including alcohol, produce intense feelings of pleasure. This initial sensation of euphoria is followed by other effects, which differ with the type of substance used. For example, with stimulants such as cocaine, the “high” is followed by feelings of power, self-confidence, and increased energy. In contrast, the euphoria caused by opiates such as heroin is followed by feelings of relaxation and satisfaction. To feel better Some people who suffer from social anxiety, stress-related disorders, and depression begin abusing substances in an attempt to lessen feelings of distress. Stress can play a major role in beginning use, abuse, dependence (addiction) and relapse. To do better The increasing pressure that some individuals feel to chemically enhance or improve their athletic or cognitive performance can play a role in initial experimentation and continued abuse. Curiosity and “because others are doing it” Adolescents are particularly vulnerable because of the strong influence of peer pressure; they are more likely to engage in “thrilling” and “risk taking” behaviors and experiment with alcohol and/or other drugs. (Source: Modified from NIDA, 2007) |
| For more information on risk and protective factors and age of first use — See Section 5 |
DSM-IV Guidelines
The American Psychiatric Association provides guidelines to diagnosing alcohol and other drug abuse and dependence (or addiction) in their Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (APA, 2000).
The diagnosis of abuse can be made when one or more of the symptoms are present at some point in the past 12 months. The diagnosis of dependence requires three or more of the seven symptomsto be present (O’Brien, 2003). Physical dependence alone (tolerance or withdrawal) is insufficient for a diagnosis of substance addiction (O’Brien, 2003; McLellan et al., 2000).
There are seven symptoms of substance dependence
- Tolerance, as defined by either:
a. need for larger amounts of the substance in order to achieve intoxication or desired effect; or
b. markedly diminished effect with continued use of the same amount
- Withdrawal as manifested by either:
a. Characteristic withdrawal syndrome for the substance; or
b. The same (or closely related) substance is taken to relieve or avoid withdrawal symptoms
- Substance is often taken in larger amounts or over a longer period than intended
- Persistent desire or unsuccessful efforts to cut down or control substance use
- A great deal of time spent in activities necessary to obtain, use, or recover from the substance
- Important social, occupational, or recreational activities are given up or reduced because of substance abuse
- Continued use despite knowledge of physical or psychological problems caused or exacerbated by the substance
Impact on the Brain
Though the initial use of substances is voluntary, continued heavy use can lead to dependence (or addiction), which is a chronic brain disease that causes physical changes in areas of the brain that are critical to judgment, decision-making, learning, memory, and behavior control. Once an individual becomes addicted to a particular substance, their actions become in part involuntary in response to their brain’s demand or craving for increased use despite medical and legal consequences. Technical violations of probation, which are frequently seen in the justice system, may be partially driven by this biological process.
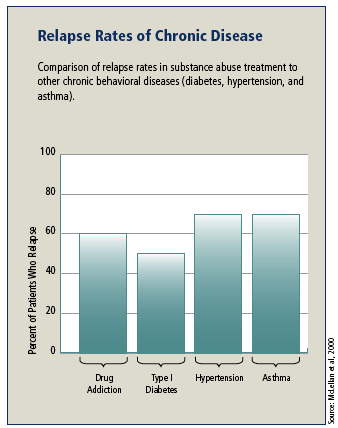
Alcohol and other drugs alter the way brain cells, called neurons, communicate with each other. Neurons send messages to each other through molecules called neurotransmitters. Examples of neurotransmitters are acetylcholine, norepinephrine, dopamine, serotonin, and GABA (gamma aminobutyric acid). Drugs disrupt the normal flow of communication in the brain in unique ways: some drugs activate receptors and others block them. Drugs, such as marijuana and heroin, can activate neurons because their chemical structure mimics that of a natural neurotransmitter, which causes neurons to respond as if the natural neurotransmitter were present. Cocaine and amphetamines block the dopamine transporter that normally removes dopamine from the synapse, the space between neurons. Both activation and blocking of receptors result in increased dopamine levels, which in turn results in feelings of euphoria.
Areas of the brain affected by alcohol and other drug use
Alcohol and other drugs have specific and long-lasting effects on the brain. Introducing alcohol and other substances during adolescence has lasting consequences because the brain is still developing.
The brain stem controls basic functions critical to life, such as heart rate, breathing, and sleeping.
The limbic system contains the brain’s reward circuit—it links together a number of brain structures that control and regulate our ability to feel pleasure. Feeling pleasure motivates us to repeat behaviors such as eating—actions that are critical to our existence. The limbic system is activated when we perform these activities—and also by substances of abuse. In addition, the limbic system is responsible for our perception of other emotions, both positive and negative, which explains the mood-altering properties of many substances.
The cerebral cortex is divided into areas that control specific functions. Different areas process information from our senses, enabling us to see, feel, hear, and taste. The front of the cortex, the frontal cortex or forebrain, is the thinking center of the brain; it powers our ability to plan, solve problems, and make decisions. Since this part of the brain is developing rapidly during adolescence, this may help explain why adolescents are more likely to engage in risky behaviors like using alcohol and other drugs (NIDA, 2007).
Understanding Relapse
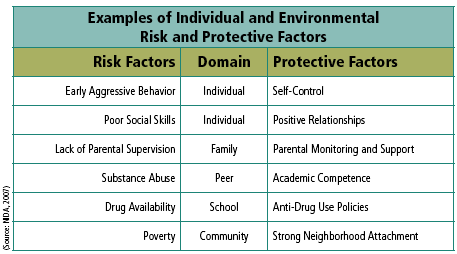
The effect alcohol and other drugs has on the brain helps explain the role of relapse involved with addiction. Relapse is a reoccurrence of substance use after a period of abstinence, often when treatment has been initiated. The justice system tends to view relapse as a voluntary violation of the law. However, relapse frequently occurs when an individual is trying to stop using a substance, but finds it to be difficult for their altered brain to resist craving.
The medical system, however, does not regard relapse as a failure of treatment. Relapse to addiction occurs at similar rates to other chronic medical conditions such as diabetes, hypertension, and asthma. Like other chronic relapsing disorders, addiction to substances may require a change in treatment until abstinence is achieved. This is similar to when a diabetic does not take their medications or fails to exercise as outlined by their physician; their non-compliance and relapse are not seen as a failure but their treatment is altered to more effectively address their problems.
Studies show that several chronic, relapsing medical conditions have high relapse rates. Alcohol and other drug treatment has a comparable or lower relapse rate than other chronic, relapsing medical conditions. Each year a recurrence of symptoms that requires medical care is experienced by 30-50% of adult patients with type 2 diabetes, 50-70% of adult patients with hypertension, 50-70% of adult patients with asthma, and 40-60% of adult patients with alcohol and drug dependence (McLellan et al., 2000). Therefore, it is important to address alcohol and other drug problems as a chronic, relapsing medical disorder and not as an acute illness. Providing programs to address relapse prevention and continuing care are important to maintaining sobriety.
Alcohol and other drugs target the brain’s reward system
All substances of abuse directly or indirectly target the brain’s reward system by flooding the circuit with dopamine. Dopamine is a neurotransmitter in regions of the brain that regulate movement, emotion, cognition, motivation, and feelings of pleasure. Dopamine pathways, known as the brain’s reward pathways, are important for natural rewards like food and sex.
Our brains are wired to ensure that we will repeat life-sustaining activities by associating those activities with pleasure or reward. Whenever this reward circuit is activated, the brain notes that something important is happening that needs to be remembered, and teaches us to do it again automatically.
Alcohol and other drugs stimulate the same reward circuit, teaching our brain to remember and desire feelings of euphoria and pleasure. These substances over-stimulate this natural system—that can release 2 to 10 times the amount of dopamine that natural rewards do. The resulting effects on the brain’s pleasure circuit dwarfs those produced by naturally rewarding behaviors such as eating and sex. The powerful reward produced by alcohol and other drugs strongly motivates people to continue use.









