PROVIDENCE, R.I. [Brown University] — A new study finds a significant racial disparity within a doubly troubled population of patients: those with HIV and Hodgkin lymphoma. In such cases, blacks are at significantly higher risk than whites of not receiving treatment for the cancer that in many cases would be effective.
“Black patients have higher rates of not receiving treatment,” said lead author Dr. Adam Olszewski, associate professor of medicine in the Alpert Medical School of Brown University and a physician in the Cancer Center of Memorial Hospital in Pawtucket, R.I. “Hodgkin lymphoma is generally believed to be highly curable. We have an expectation to cure over 90 percent of early stage patients and even 70-80 percent of quite advanced cases.”
Olszewski’s study in the journal AIDS, conducted with Dr. Jorge Castillo of Dana-Farber Cancer Institute, identified the racial disparity in data from nearly 2,100 cases in the National Cancer Data Base between 2004 and 2012.
While the disparity is clear, Olsewski said, the root cause of it is not. Several closely entangled epidemiological, socioeconomic, and medical factors are at play.
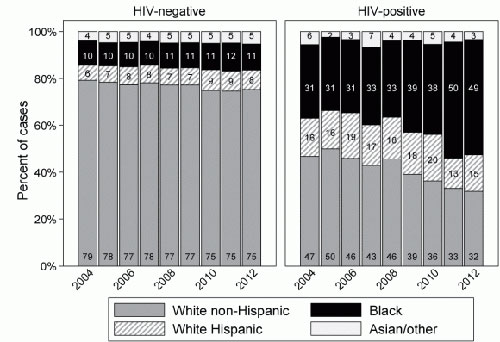
Heading into the study, researchers knew that people with HIV have a risk of Hodgkin lymphoma that is five to 20 times greater than people who do not have HIV. They also knew that HIV incidence has remained relatively high among blacks, while it has dropped significantly for whites. As a result, the new study found that between 2004 and 2012, blacks surpassed whites as the largest racial group with simultaneous HIV infection and Hodgkin lymphoma, making up 49 percent of such cases in 2012.
Meanwhile, doctors have had a muddy sense of whether HIV-positive people with Hodgkin lymphoma survive the cancer as well as people who are HIV-negative. Many HIV-positive patients didn’t tolerate an older treatment regime for the lymphoma, Olszewski said, but chemotherapy treatment has vastly improved in more recent years. While some small studies, particularly in Europe, have found that HIV status makes no difference to survival, observations in the U.S. population suggest that being HIV-positive makes survival less likely.
The new study, the largest to date, may reconcile that conflict. It shows that in the United States the reason people with HIV seem to fare worse with the cancer is because they are less likely to be treated for it.
Specifically, the study ostensibly showed that HIV-negative people had an 80 percent Hodgkin lymphoma survival rate five years after diagnosis, but HIV-positive people survived at a rate of only 66 percent over the same timeframe. But among HIV-positive patients, 16 percent went untreated. Among people in the study who did get lymphoma treatment, HIV-positive people were statistically just as likely to survive as HIV-negative people. The results apply to the majority of cases in which the subtype of Hodgkin lymphoma is determined.
Importantly, further statistical analysis showed that one of the main risk factors for an HIV-positive person going untreated was being black. Statistically adjusting for possibly confounding factors, HIV-positive blacks were 67 percent more likely than HIV-positive whites to go untreated for the lymphoma. Other risk factors, which are often related to race, were low income and lacking health insurance. Another was being over 60 years of age.
Olszewski acknowledged it’s not clear how the racial disparity arises. It could correlate with more advanced or poorly controlled HIV infection. It could also be a lingering assumption that HIV-positive patients (who are increasingly likely to be black) won’t tolerate the treatment well. Some patients may be declining treatment, either for HIV (thereby making them seem more vulnerable) or for the lymphoma itself. Another possibility is that the often-related socioeconomic status of being black and poor and uninsured makes it hard for patients to remain connected to care after diagnosis.
For patients who have HIV and Hodgkin lymphoma, treatment can be effective and tolerated, especially when the lymphoma subtype is known, Olszewski said, but doctors should understand that some patients many need extra assistance or attention to ensure they connect with that care.
To date, his study suggests, it’s apparent that some people who should get treatment aren’t getting it.