PROVIDENCE, R.I. [Brown University] — For cancer to spread, the cells that take off into the bloodstream must find a tissue that will permit them to thrive. They don’t just go looking, though. Instead, they actively prepare the tissue, in one case by co-opting a protein that suppresses defenses the body would otherwise mount. In a new study, scientists report that by wresting back control of that protein, they could restore multiple defenses in the lungs of mice, staving off cancer’s spread there.
“Cancers are known to have the ability to co-opt or evade host anti-tumor responses,” said Dr. Jack A. Elias, dean of medicine and biological sciences at Brown University and corresponding author of the study in the Nature journal Scientific Reports.
A key protein that apparently becomes co-opted is Chitinase 3-like-1 (CHI3L1), which has a natural purpose in a wide array of organisms where it helps to fight infections and stimulates tissue healing. However, it is also susceptible to going awry where it contributes to the generation of a variety of diseases. In human diseases like idiopathic pulmonary fibrosis it mounts an overzealous response that leads to pulmonary scarring, and in diseases like asthma it sustains a harmful immune response. People have a directly analogous version of the protein called YKL-40 and, in patients with cancer, high levels of its expression correlate strongly with advanced cancer spread and a poor prognosis
Ina 2014 study, Elias’s team at Brown and Yale found evidence that CHI3L1 has a central role in making tissues receptive to cancer spread.
“It seems to be a very fundamental pathway,” said Elias, a specialist in pulmonary medicine and immunology. “It’s not a pathway that’s just in this disease or that disease. It’s a fundamental way that the body responds, and as a result it has many different consequences.”
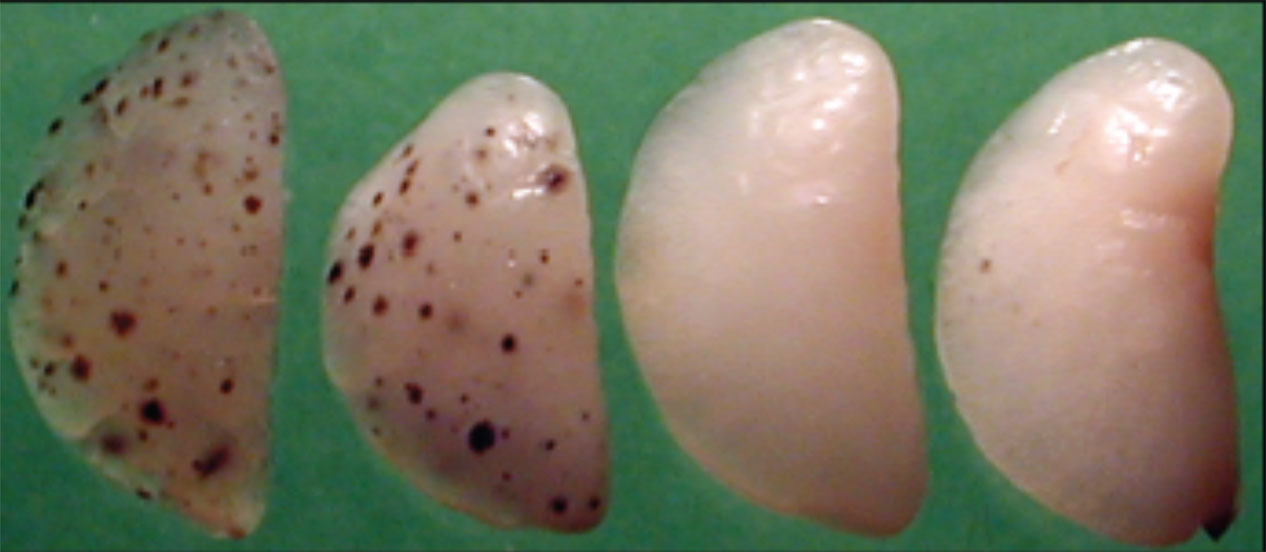
In the new study, the researchers not only explained more about how CHI3L1 promotes cancer spread but they also tested a new intervention that had especially widespread effects. The scientists exposed mice to melanoma or breast cancer cells and then treated different mice at different times over the next eight days to suppress expression of CHI3L1. In treated mice they restored several mechanisms that the body has to fight tumors and were able to prevent the lungs from becoming hospitable to the cancer. Mice left untreated as experimental controls quickly developed cancer in their lungs after exposure to cancer cells.
Restoring defenses
Several experiments revealed the details of what was going on in the lungs of the mice. They defined a pathway that contributes to cancer spread by stimulating CHI3L1, a novel pathway that blocks CHI3L1 and cancer spread,, and highlighted the ways that tumors evade this antitumor response.
In the presence of cancer, for example, a protein called semaphorin 7A induces the expression of CHI3L1, which blunts a number of antitumor responses including those initiated by natural killer cells and a protein called PTEN. These studies also demonstrated that activation of a novel antiviral immune response pathway called the RIG-like helicase (RLH) pathway counteracts the ability of cancer cells to stimulate CHI3L1 and decreases the tumor-inducing effects that it mediates. Furthermore, they demonstrated that cancer cells stimulate another protein called NLRX1, which suppresses the RLH response that allows tumor cells to induce CHI3L1. Thus, Elias said, cancer cells stimulate CHI3L1 while simultaneously using NLRX1 to suppress the CHI3L1-inhibiting effects of the RLH pathway.
The new intervention that Elias’s team tested was to bolster RLH immunity by stimulating its pathway with an RNA-like molecule called Poly(I:C). In mice this intervention reduced CHI3L1 production and its cancer-augmenting responses. While untreated mice went on to develop cancer in their lungs within two weeks, mice given Poly(I:C) fended the cancer off. Notably, among the effects was an increase in natural killer cells, natural killer cell recruiting proteins, stimulation of the proteins LIMK2 and PTEN and suppression of B-Raf and Nlrx1proteins. Recently scientists have attempted to develop cancer-fighting drugs by focusing on some of these individual proteins, but not multiple ones at the same time.
“What we show in this paper is there is a very novel pathway, the RLH pathway, that can actually control the production of CHI3L1,” Elias said, “and when you can control the production of CHI3L1, you can control each of these pathways, and you can control the spread of cancer in these models”
In several of the experiments the team didn’t just compare treated mice with untreated mice. Often they also used the additional controls of mice engineered to lack the gene that produces a particular protein, like CHI3L1. These steps helped to test whether the particular protein being investigated really played the suspected meaningful role.
It was clear that giving RLH the upper hand against CHI3L1 proved meaningful for suppressing cancer spread in the lungs of the mice.
“The thing that’s exciting is that [stimulating the RLH pathway] is going to allow multiple antitumor response to be augmented vs. just one,” Elias said. “If you can agonize the RLH pathway, you might get a really good effect in cancer.”
The study’s lead author is Bing Ma, assistant professor of molecular microbiology and immunology at Brown. The paper’s other authors are Erica Herzog, Meagan Moore, Chang-Min Lee, Sung Hun Na and Chun Geun Lee.
The National Institutes of Health (grants: R01HL093017, UH2HL108638, R01HL115813, HL109233, HL125850) and the Korea Drug Development Fund (KDDF-20132-11) supported the research.