A healthy human liver cell. The hepatitis C virus attacks the liver, leading to damage that progresses to cirrhosis, liver failure or liver cancer. Donna Beer Stolz, University of Pittsburgh
PROVIDENCE, R.I. [Brown University] — On the eve of a WaterFire celebration dedicated to eliminating hepatitis C, a new Brown University study projects that increasing the number of Rhode Islanders treated every year for hepatitis C virus infection (HCV) to about 2,000 by 2020 would reduce cases by 90 percent and prevent more than 70 percent of expected liver-related deaths in the state by 2030.
More moderate increases in treatment such as doubling the number treated each year could reduce death rates by less than 20 percent, the analysis showed.
“Hepatitis C virus-related morbidity and mortality can be reduced significantly in Rhode Island if an aggressive treatment strategy is implemented over the next decade,” wrote public health Assistant Professor Brandon Marshall and colleagues in the journal Epidemiology and Infection.
“The medications available today are so effective that — with increased treatment uptake — we have the opportunity to all but eliminate the disease by 2030,” he added.
Marshall’s analysis comes as Rhode Island takes a deep look at the how the disease has impacted the state. July 28 was World Hepatitis Day. The Aug. 6 WaterFire marks that occasion. Meanwhile, next week the Rhode Island Department of Health plans to unveil an epidemiological report, in partnership with the Rhode Island Public Health Institute, describing key aspects of the state of the epidemic.
Hepatitis C can take decades to cause serious disease, but ultimately the liver damage it can cause can be fatal as it progresses to cirrhosis, liver failure or liver cancer. In recent years many baby boomers (infected as long ago as the 1950s, ’60s and ’70s) have been reaching those critical later stages of progression. One in 30 baby boomers in the U.S. has hepatitis C. At the same time, new treatments have made the disease curable in only a few weeks, very safely, but in the U.S. they are priced at tens of thousands of dollars.
“Hepatitis C kills more people in the United States than any other infectious disease,” said study co-author Dr. Lynn E. Taylor, assistant professor of medicine, physician at The Miriam Hospital and founder of Rhode Island Defeats Hepatitis C. “In fact, hepatitis C causes more deaths than all other 60 infectious diseases reportable to the CDC, combined. This is the critical infectious disease epidemic of our time. Our goal is elimination. We need to scale up our testing and treatment with urgency to avert preventable illness and early death.”
Modeling mortality
The new study sought to project the impact of expanding treatment by varying degrees using a sophisticated computer model loaded with data from Rhode Island’s epidemic or, when that data wasn’t available, from that of the U.S. more broadly.
Marshall’s team, including lead author and Brown public health graduate student Dr. Ayorinde Soipe, included figures and estimates for the number of Rhode Islanders infected since 1950, the progression rate of hepatitis C’s various strains and the rate of new infections. They also considered many other pertinent factors including how often people die of the disease vs. other causes over time, and the likelihood that they could clear the infection without treatment.
They then used the model to project the course of the next 14 years of the epidemic in Rhode Island based on four different treatment scenarios:
- The Base Case: Treatment for 215 residents a year, restricted to patients with stage three fibrosis or worse.
- Scale-up 1: Double treatment to 430 residents annually and treating patients with stage two fibrosis or worse.
- Scale-up 2: Double treatment to 430 residents annually and treating patients irrespective of HCV disease stage.
- The “Elimination” Scenario: Whatever the model says is needed to reduce infections by 90 percent by 2030, which turned out to be treating 2,000 patients a year by 2020.
The greatest reductions in liver-related deaths by 2030 occurred in the elimination scenario: a drop of 72.4 percent compared to the base case.
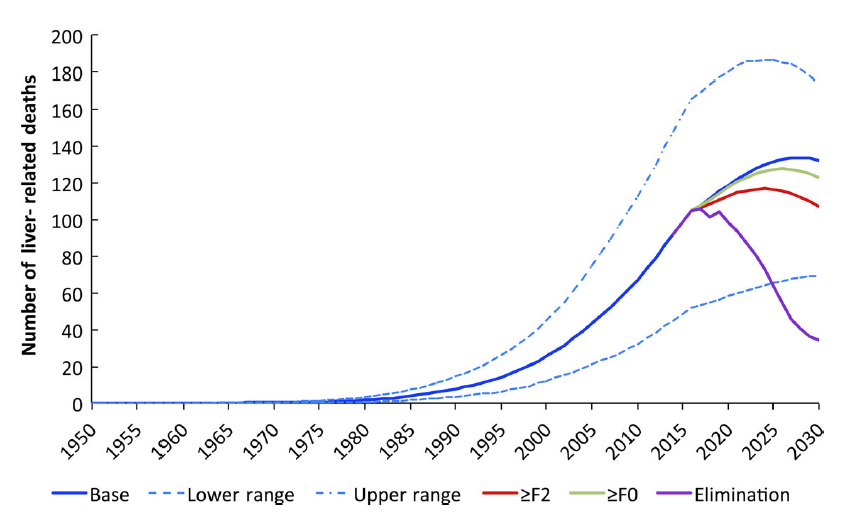
Projections show that the "elimination" strategy could dramatically reduce liver-related deaths in Rhode Island over the next decade and a half.
Brandon Marshall, et. al.
Scale-up 1 would reduce liver-related deaths by 19.3 percent, and Scale-up 2 would reduce them by 7.4 percent.
Similar patterns of reductions would also bring down the number of cases of cirrhosis, which could lead to more deaths after 2030.
Marshall said that the reason why maintaining a restriction on treating patients with more advanced liver disease would result in fewer deaths (as in Scale-up 1 vs. 2) is because with few people being treated, it would prevent more deaths if treatment resources were focused on those more acutely ill.
The study did not track the costs of expanding treatment, which would likely be in the tens of millions of dollars. The researchers noted, however, that while the upfront investment would be large, it would likely pay off eventually in preventing thousands of cases of cirrhosis, liver failure and liver cancer, which are expensive to treat and would drastically reduce the need for very costly liver transplants.
The study has other limitations, such as the need to make assumptions based on national rather than state data. It also might underestimate the prevalence of hepatitis C because it does not account for rising infection rates among young people amid the state’s opioid and heroin epidemic.
Still, Marshall said, the study provides guidance for state policymakers, insurers and care providers about what it will take to bend the curve of the state’s epidemic to result in far fewer deaths.
In addition to Soipe, Marshall and Taylor, the paper’s other authors are Brown public health Assistant Professor Omar Galárraga and Drs. Homie Razavi and Devin Razavi-Shearer of the Center for Disease Analysis in Lafayette, Colorado.
The Rhode Island Foundation’s support of R.I. Defeats HepC funded the research. Dr. Soipe was supported by a trainee award from the Lifespan/Tufts/Brown Center for AIDS Research (CFAR), and Dr. Marshall is supported by a Henry Merrit Wriston Fellowship from Brown University.