
PROVIDENCE, R.I. [Brown University] —Since Dr. Adam Levine arrived in Haiti in late October, he’s been managing a cholera treatment unit for International Medical Corps. Hurricane Matthew devastated the area on Oct. 4, creating conditions that foment the spread of the disease. The unit is still running near its 30-bed capacity.
The unit is a pair of tents on the grounds of a local health center in Les Anglais, said Levine, an associate professor of emergency medicine at Brown University and a physician at Rhode Island Hospital. The town sits almost at Haiti’s western tip on the southwest shore of its southern peninsula.
Levine, who directs the new Humanitarian Innovation Initiative at Brown’s Watson Institute for International and Public Affairs, answered questions about his work providing life-saving rehydration and medicine to people who make a difficult trek to the center from surrounding villages.
Tell us about the cholera epidemic in Haiti in the wake of Matthew.
Our 30-bed unit runs pretty full on most days, and we probably get about 10 to 15 new patients each day. Most of the cases coming from the small villages and towns of the department we are in. We generally see the sickest patients who are able to make it to our treatment unit. They have traveled quite far to get here. They have to walk down from their village in the hills to the nearest road to catch a motorcycle that can bring them here.
We’re probably seeing just a small proportion and just the sickest patients. We know that there are many more in the surrounding area. International Medical Corps. has been setting up oral rehydration points — sending someone up to a village with a backpack with oral rehydration stations and basic medicines and supplies. They set up an oral rehydration point there so they can at least treat mild or moderate cases in the village and only have to send the most severe cases to us because transport is so difficult.
How are you treating cholera?
Cholera treatment is relatively straightforward, but it’s important to stick to the protocols very carefully. A cholera patient can lose up to 10 to 15 liters of water a day from profuse diarrhea — it can actually kill patients within 24 hours just from severe dehydration. So the most important aspect of treatment is providing adequate rehydration either with oral rehydration solution or, for those who are more severe, with intravenous fluids. There is also an antibiotic that we use. It decreases the length of the course of cholera.
The complicated part of running a cholera treatment unit is that cholera is very contagious and you don’t want to spread it. We need to pay very close attention to infection prevention and control. That’s why we treat patients in a separate unit instead of in the hospital.
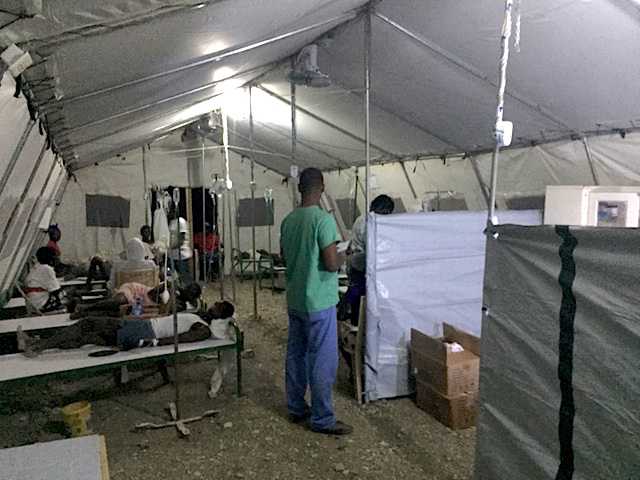
Can you describe what the treatment unit is like?
In the back of the health center, we’ve cordoned off an area with fencing so that nobody comes in or out except for patients and staff. Within that cordoned-off area, we’ve set up two tents. One of the tents is for treating patients with severe dehydration with IV fluids. The other is for treating patients with oral fluids for moderate dehydration. Patients will come into a small triage area and nurse’s station where we evaluation them and confirm whether they have cholera. If they do, we assess how severe their dehydration is.
Usually cholera resolves in a few days, or a little bit faster if you use the antibiotic. When they are feeling better and are totally rehydrated and no longer have diarrhea and vomiting — and therefore are no longer infectious — we will have them take a chlorine shower and discharge them.
Usually a patient comes in with a family member or a caretaker. They help take care of them inside the unit so we also have to make sure that caretakers wash their hands frequently and do not put themselves at risk.
From what you see around you, are the resources there enough to meet the need?
Haiti is the poorest country in the Western Hemisphere and its health care system is underdeveloped as a result of that. In Les Anglais, the health center is staffed by one doctor and a few nurses. They have limited medical supplies and limited diagnostics and treatment that they can provide. They do the best that they can with what they have. But this health center is hard for many patients to reach because they live up in the hills where there are no roads.
This is a problem in the best of times. But now we’re in the aftermath of a natural disaster, and we know that people are displaced from their homes and living in more crowded conditions. Maybe they are living with family members because their home was destroyed. A lot of people in surrounding communities have been sheltering in schools.
You know there are a lot of people living together and it’s easier for cholera to be transmitted quickly from one patient to the next. The hurricane didn’t cause cholera. Cholera has been in Haiti for six years now. But the hurricane caused conditions that make the spread of cholera easier. That’s why we are seeing more cases.
As you perform your clinical work, are there research questions on your mind, too?
I always have research in the back of my mind. Much of my research focuses on assessment and management of dehydration in patients in Bangladesh. Working in an actual cholera treatment unit in the field definitely makes me understand and realize a lot of technical aspects of cholera management. It makes me think more about the ways you can help clinicians — nurses and doctors in the field — in poor countries who respond to these types of outbreaks. Are there better tools we could give them? How can we make their lives simpler and easier?
One example is that the treatment guidelines for cholera are pretty simple, in theory — there are specific amounts of fluids and medicine based on patients’ needs. But then when you actually try to implement that, you realize that (a) they don’t have a scale in the health center, so they are not able to actually weigh the patient; and then (b) they don’t have calculators, and it’s not easy to calculate 70 ccs (of fluid) per kilo (of weight). Nor is it easy when you don’t have an automated IV pump to type in how many milliliters you are going to give over an hour. You have to do it by counting the drips from the IV.
So one of the studies that I’m going to be doing next April in Bangladesh is looking at a mobile phone based app that can help clinicians figure out exactly how dehydrated the patient is just by typing in the symptoms — and then also help them figure out how much fluid to give a patient and how many drips per minute they have to give. It’s those implementation questions that I think are most interesting.