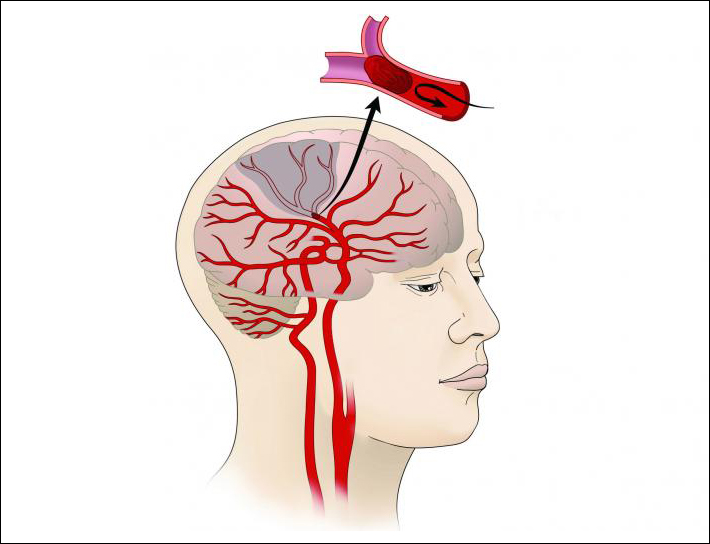
PROVIDENCE, R.I. [Brown University] — As soon as possible after a stroke, a critical step is to eliminate the clot that caused it. While the current standard of care is to use “clot busting” tissue-type plasminogen activator drugs, recent studies have shown greater medical efficacy in combining the drugs with a “stent retriever” that mechanically opens the artery for a device to grab it and pull it out — a surgical procedure called “thrombectomy.”
The question remained, however, of whether the added procedure was cost-effective. A new study co-authored by Theresa Shireman, professor of health services, policy and practice at the Brown University School of Public Health, found that it is. After higher initial costs, Shireman explains in the interview below, better outcomes for patients make stroke-related care less costly in the long run.
Shireman was lead author of the study published in the journal Stroke.
To compare the cost-effectiveness of one treatment vs. another, what did you measure?
In general, new technologies or treatments in health care cost more than the existing standard of care. In cost-effectiveness analysis, the purpose is to judge the relative increase in costs against the presumably improved benefit or effect. There are occasions, however, where a new treatment provides greater benefit or effect at a lower cost. That is the case with the technology we analyzed.
How much more cost effective was treatment with the mechanical thrombectomy plus the drug than treatment with the drug alone?
In the case of the technology we assessed, it made the initial hospitalization for ischemic stroke more expensive (the cost of actually doing the procedure) but patients improved so much in their stroke recovery that long-term costs were lower. In other words, patients' recovery with respect to physical function was so much better with stent retriever thrombectomy that they were less likely to need nursing home rehabilitation and longer nursing home care. This saved money so that within 22 months, the higher procedure costs had been covered.

Does cost-effectiveness (rather than care effectiveness) matter to patients and their families or only to insurers and providers?
Cost-effectiveness should matter to all of us, as it is one approach to finding the most efficient health care interventions — those that generate the greatest benefit at the lowest cost. If we regularly find the most efficient interventions, we all will pay less for health care and have the best outcomes. In the case of stent retriever thrombectomy, it is easy to see the patient and family benefits, as they have better functional recovery post-stroke and are less likely to need nursing home care. That’s a double-win for them and for payers and providers. In many cases, however, cost-effectiveness analyses may not generate such clear results, and not all analyses adhere to consensus guidelines.
How might these findings affect stroke treatment in the future?
For patients who suffer an ischemic stroke and are located close enough to a stroke center or hospital with the appropriately trained interventionist, access to stent retriever thrombectomy should be able to dramatically reduce the burden of stroke.
What was your role in the study?
The project was designed by Dr. David Cohen and his team at the Saint Luke’s Mid-America Heart Institute in Kansas City, Missouri. I served as the lead investigator, shepherding the project through its various phases, reviewing intermediate steps, presenting the findings at an international conference and preparing the final manuscript.
Editor’s note: Medtronic, which makes the stent retrieval device, funded the study.