PROVIDENCE, R.I. [Brown University] — At the beginning of the 2017-18 academic year, Dr. Neel Sodha, a cardiothoracic surgeon, walked into a classroom full of Brown University engineering students and presented them with a problem.
While cardiac bypass surgeries save hundreds of thousands of lives every year, some patients are at risk of neurological damage following the procedure, as plaques and other debris break loose from the heart and travel to the brain. Around 10,000 people nationwide suffer these embolic strokes every year. The devices available to heart surgeons aimed at preventing these strokes — aortic filters designed to capture debris before it exits the heart — simply don’t work as well as doctors would hope. Dr. Sodha, who is on the faculty of Brown’s Warren Alpert Medical School, challenged the students to come up with something better.
A team of five students from the class — a senior capstone course required for all Brown biomedical engineering concentrators — took up that challenge. Over the course of the fall semester, the students designed a new aortic filter, built a prototype and performed computational and benchtop tests to assess the safety of the device and its efficiency at capturing embolic debris without impeding blood flow. Their testing suggests that their device, dubbed Embonet, is effective at capturing and holding embolic debris while allowing blood cells to pass through. The team has filed a provisional patent for its design, and last spring the device won first prize in the Advanced Healthcare Systems track at the 2018 Johns Hopkins International Healthcare Design Competition. The team is currently exploring commercial options for its idea and hopes to license the technology to a medical device company.

Embonet is exactly the kind of innovative project addressing a real-world need that engineering faculty members Anubhav Tripathi and Celinda Kofron had in mind when they designed the capstone course. The semester begins with a series of presentations by clinicians describing clinical needs. The students then form teams around a particular problem and work for the remainder of the semester on a solution. This is the second year that the class has been structured in this way. Next year, it will transition from a one-semester course to a full-year requirement.
“The idea behind the class was to reach out to practitioners — people working in the field who have firsthand knowledge — and let them give us the problems,” said Tripathi, a professor in the School of Engineering. “By the end of the semester, we would like see students come up with a proof of concept for a solution and a realistic attempt at a prototype. Students can’t just turn in a paper and get a grade. This is about innovation.”
In the process of developing their solutions, students are guided by relevant engineering and design concepts drawn from material science, biophysics, biomechanics and other areas. But it’s the real-world problems and the direct mentorship from clinicians in the field that makes the class particularly effective, says Kofron, an engineering lecturer who co-teaches the course with Tripathi.
“Anubhav and I facilitate this, but there’s no way we could be experts in all these fields,” Kofron said. “Our clinical participants provide that knowledge base. Brown is in the perfect place to do this because we’re well so connected with the medical school and with clinicians at Rhode Island Hospital, Women and Infants and other hospitals.”
Ileana Pirozzi, a Brown senior who graduated in May, was a member of the Embonet team along with classmates Berke Buyukkucak, Celina Hsieh, Emily Holtzman and Gian Ignacio. Pirozzi says that the problem-based approach and the chance to work side-by-side with a surgeon — including observing surgical procedures — made for an invaluable educational experience.
“As a biomedical engineer, it’s really about bridging that gap between the engineering side and the medical side,” she said. “In order to effectively build that bridge, engineers need to know how to communicate with the doctors. In other words, we need to become fluent in the language of medicine and understand the priorities of the operating room and the shortcomings of current technologies. Being able to sit in on surgeries, and to look at existing medical devices to understand why they’re failing … was really something you can’t get in just the four walls of a classroom.”
Embonet isn’t the only project to emerge from the course with real commercial potential. Nor is it the only one to be recognized at a major biomedical design competition.
Another team from the class designed a system to aid in the implantation of electrodes used in deep brain stimulation (DBS), a technique used to treat Parkinson’s disease and other movement disorders. DBS involves placing electrodes into the brain that deliver a small electrical current, which helps to regulate abnormal brain activity. Current DBS systems don’t allow much flexibility in how they operate; they’re either on or off. Ideally, however, clinicians envision more advanced systems that can sense a patient’s brain activity at any given moment and adjust the current they deliver accordingly.
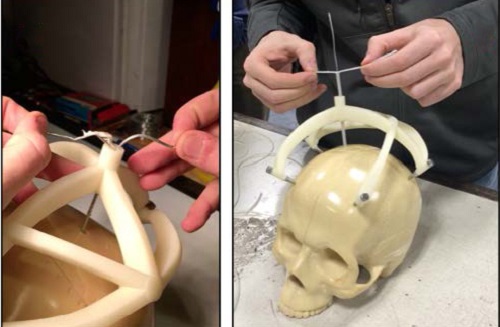
Prototypes of such two-way DBS systems exist, but they’ve not yet been used in clinical trials. One potential reason is that more complex electrode systems are incompatible with current surgical equipment — specifically the guide tubes used to place electrodes inside the brain. That problem was presented to the capstone class by Dr. Wael Asaad, a professor of neurosurgery at the Alpert Medical School. Owen Leary, Rohan Rastogi, Zakir Tahiry and Noah Trac took up the challenge and designed a new surgical guide tube that can accommodate more complex electrode arrays. The design won first prize in the Image and Signal Acquisition category of the Northeast Bioengineering Conference, a regional competition at Drexel University last April.
Leary, who graduated in May and is on his way to Alpert Medical School under Brown’s Program in Liberal Medical Education, says that working with both Dr. Asaad and Shane Lee, a postdoctoral researcher in Asaad's lab, was critical to the design process.
“[Dr. Asaad] allowed us to go into the operating room and see the surgery for ourselves,” Leary said. “That really helped us to conceptualize the procedural bottleneck that seems to be preventing the implementation of more complex current exchange systems in DBS.”
The team holds two preliminary patents on their design, and Leary is taking a year off before he starts medical school to pursue the idea further. He says the class gave him a new perspective on the field of biomedical engineering.
“It helped me to understand what biomedical engineering is all about,” Leary said. “Actually having the opportunity to try your hand at designing a real device that might get translated to patients — and to have it discussed in an entrepreneurial framework — has been unique in my experience so far.”
But it’s not just the students who come away from the experience with something beneficial. The clinical advisors who work with the class see the value as well. Dr. Ravi D’Cruz, a fellow in neonatal and perinatal medicine at the Brown-affiliated Women and Infants Hospital, has served as a clinical advisor for the class since 2016, the first year that the problem-focused format was used. He’s overseen five projects from the class over the last two years.
“It’s really nice as a clinician to be able to bring people into your space,” D’Cruz said. “The neonatal intensive care unit is so specialized. It is its own little arena with its own language. But to be able to bring students in there and have them fully immerse themselves is a really great thing. By the end, they really understood the problem inside and out.”
D’Cruz worked with a group of students who created a new kind of transilluminator, the device doctors use to help find veins for blood draws and other procedures. The transilluminators currently on the market are maddeningly unwieldy, he says. Doctors are constantly fumbling with them and dropping them. The undergraduate team at Brown devised an idea for a wearable transilluminator that’s much easier to use. The students are hopeful they’ll be able to license the idea to a medical device maker.
D’Cruz said he was impressed with what the students in the class had to offer and how the design of the course led to innovative ideas.
“I used to be an architect before going into medicine, so I had this background knowing that there are things that are fixable through design,” D’Cruz said. “But one of the biggest issues I see is that we build up silos where designers aren’t privy to the problems in health care, and the people who can identify the problems in health care don’t know how to fix them through design. So it’s nice to have a way to bring those two sides together.”
The innovative projects have emerged from the class so far, several with real commercial potential, show just what can happen when those two sides meet.