PROVIDENCE, R.I. [Brown University] — Supported with a new grant of $6.3 million from the U.S. Defense Advanced Research Projects Agency (DARPA), a team led by Brown University researchers will develop and test an “intelligent spinal interface” aimed at helping to restore limb movement and bladder control for people who have suffered spinal cord injuries.
Developed in collaboration with physicians at Rhode Island Hospital, a Lifespan partner, along with commercial partners at Intel and Micro-Leads Medical, the experimental spinal interface will be designed to bridge the gap in neural circuitry created by a spinal injury, the researchers say. The idea is to record signals traveling down the spinal cord above an injury site and use them to drive electrical spinal stimulation below the lesion. At the same time, information coming up the cord from below will be used to drive stimulation above the injury. The device could potentially help to restore both volitional control of limbs muscles as well as feeling and sensation lost due to injury.
“We know that circuits around a spinal lesion often remain active and functional,” said David Borton, an assistant professor at Brown’s School of Engineering and a researcher at the University’s Carney Institute for Brain Science who will lead the project. “The hope is that by using information from either side of a lesion in a bidirectional way, we could make a significant impact on the treatment of spinal cord injuries. This exploratory study aims to build the toolset — the mix of hardware, software and functional understanding of the spinal cord — to make such a system possible.”

Over the next two years, the research team will work with Dr. Jared Fridley and the neurosurgery staff at Rhode Island Hospital to recruit volunteers with spinal cord injuries to be implanted with an experimental interface for a period of up to 29 days. The device will record and stimulate the spine as patients participate in standard physical therapy for spinal injuries.
“This is truly a transformational effort that has the potential to have a significant impact in the lives of patients with spinal cord injury, particularly for our veterans with war-related spinal cord damage,” said Dr. Ziya Gokaslan, neurosurgeon-in-chief at Rhode Island and Miriam hospitals, clinical director of Lifespan’s Norman Prince Neurosciences Institute and chair of neurosurgery Brown’s Warren Alpert School of Medicine at Brown. “We are very excited to be a part of this very innovative research, which is the result of partnership between the brilliant scientists led by Dr. Borton at Brown and our team at Rhode Island Hospital as well as our industry collaborators. We are grateful for the funding of this work by the Department of Defense through DARPA and for all the support we have received from Lifespan and Brown University leadership.”
The researchers will focus on signals related to control of the legs for walking and standing as well as signals related to bladder control, the latter of which is the number one concern reported by people with spinal cord injuries. By the end of the two-year project, the researchers hope to demonstrate that the device can properly target the neural circuits that influence these activities.
“We hope that by exploring what signals are generated by the spinal cord, how they relate to activities of daily living and how electrical modulation of the spinal cord impacts these signals, we will inform future designs of therapeutic technologies,” Borton said.
Recent research by led by Borton and by teams in the U.S. and Switzerland have shown that spinal cord stimulation can help in restoring voluntary muscle control after spinal injury, potentially aiding in rehabilitation. This new project aims to build on the success of prior efforts by using signals from the spinal cord to drive stimulation in a way that more closely resembles natural signaling processes. And by making the stimulation bi-directional, it could also aid in the recovery of sensations from limbs and muscles below the injury site, as well as evolve its stimulation profile over time.
“What’s new in this project is taking information from the spinal cord itself and to use that to drive stimulation to another part of the spinal cord,” Borton said. “In this way, we’re taking advantage of as much intact tissue as we can, which we think could lead open the door to wider therapeutic application of spinal cord stimulation, for example, bladder control.”
A key portion of the project is developing artificial intelligence (AI) and machine learning tools to decode spinal signals recorded from the spine. For that, the Brown team will work with researchers from Intel, which will provide hardware, software and research support for the project. Through projects like the BrainGate collaboration, Brown researchers have done pioneering work in this area, and this new project will build on that success.
“As a Ph.D. student at Brown, I investigated how to interface the brain with machines as an application,” said Naveen Rao, corporate vice president and general manager of the AI Products Group at Intel. “Now at Intel, we’re combining our AI expertise with Brown University’s cutting-edge medical research to help solve a critical medical problem: how to reconnect the brain and spine after a major spinal injury.”
Thomas Serre, an associate professor of cognitive, linguistic and psychological sciences at Brown, will work with the AI team from Intel. As an expert in computer vision, Serre brings expertise in using an understanding of a biological system in designing artificial analogs.
“Our goal is to figure out mathematical abstractions that we can then integrate with modern machine learning architectures,” Serre said. “The hope is that if we can design our models with some knowledge of how the spinal cord works, we can develop systems that are efficient, generalizable and can learn with less training.”
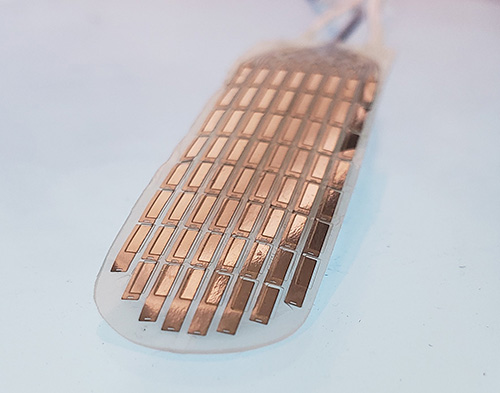
The project will make use of a high-resolution spinal cord stimulation technology developed by Micro-Leads, called HD64.
“For many years, spinal cord stimulators have led to unpredictable clinical outcomes due to an inherent difficulty with localizing therapy to only the parts of the body that need it,” said Bryan McLaughlin, founder and chief executive officer of Micro-Leads Medical. “We developed HD64 to provide a two-times increase in the number of therapy locations and greater pinpointing accuracy without changing the implantable device size or number of wires.”
In this first two-year phase of the project, the device will make use of an external computer system to decode spinal signals. However, the team hopes this project will lay the groundwork for a fully implantable device for long-term use during rehabilitation and beyond.
“We’re confident that what we learn in this program will inform future refinement of a system that will have a real impact on rehabilitation from spinal cord injuries,” Borton said.
“Lifespan and Rhode Island Hospital are proud to collaborate with Brown University and tech industry partners on this breakthrough technology and treatment endeavor, at the leading edge of neurosciences research,” said Timothy J. Babineau, M.D., president and CEO of Lifespan. “Our deep commitment to the neurosciences and to advancing clinical research compels our investment in this exciting work, and no group of physicians could be more suited to this work than our world-renowned neurosurgery team .”