PROVIDENCE, R.I. [Brown University] — In a highly anticipated announcement, the U.S. Food and Drug Administration on Monday, June 7, approved the first new drug for Alzheimer’s disease in nearly two decades.
That approval was not without controversy. Both before and after the FDA’s decision, physicians and researchers expressed a wide variety of perspectives on the drug’s potential, given a limited evidence base, and multiple stops and starts in its development and approval process.
The drug, called aducanumab during development and clinical trials, will be branded and sold as Aduhelm. Dr. Stephen Salloway, a Brown University professor of neurology and psychiatry, has been closely involved with its clinical development since the beginning.
“I really believe this kicks off a new era in the fight against Alzheimer’s disease,” said Salloway, who directs the Memory and Aging Program at Butler Hospital and has been researching Alzheimer’s disease for 30 years.
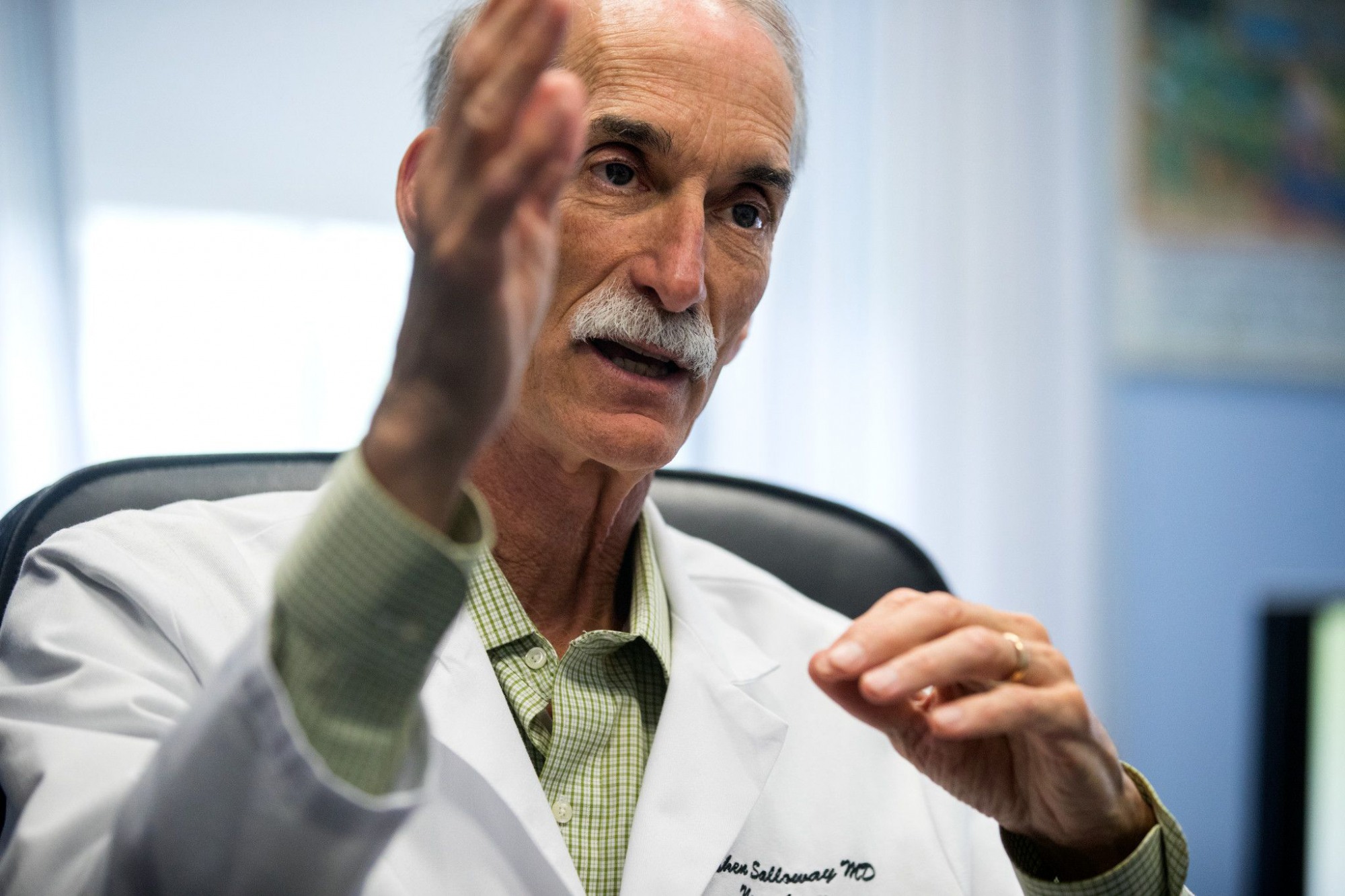
Salloway was a site principal investigator at Butler for both Phase 1 and Phase 3 trials of aducanumab, co-chair of the investigative steering committee for the Phase 3 program, and has advised the drug’s manufacturer, Biogen, on safety protocols and side effect management. He shared his perspective on what the FDA approval means for Alzheimer’s patients as well as for future research of this disease — including at the new Center for Alzheimer’s Research at Brown, a collaboration between the Carney Institute for Brain Science and Division of Biology and Medicine for which Salloway will serve as associate director.
Q: How is aducanumab different from other Alzheimer’s treatments?
It’s important to know that this is the first drug that targets a core component of Alzheimer’s disease: the amyloid plaques that play a key role in memory loss. Aducanumab is a monoclonal antibody made from the immune cells of older people with no cognitive decline or uncommonly slow cognitive decline. It binds to the amyloid plaques and breaks them up. The other drugs for Alzheimer’s focus on neurotransmitters; they alter different chemicals in the brain to help improve functioning, but they don’t really address the underlying pathology of the disease. Aducanumab is also different in that it’s an immune-based treatment that needs to be administered intravenously on a monthly schedule, ideally in a hospital-based infusion center. The treatment should be overseen by a specialist who is familiar with the patient and their diagnosis, as well as familiar with the medicine and the management of potential side effects.
Q: Why did the FDA review and approval process include so many delays?
The development of this drug started out looking very promising. The Phase 1 trial demonstrated that the drug lowered levels of amyloid in the brain, and there was some evidence of it slowing cognitive decline. Then we enrolled participants in Phase 3 larger trials to confirm that early data, and we found that it was safe to increase the dose for participants carrying the APOE4 gene for Alzheimer’s. We made a dose change for two-thirds of the study participants, and that affected how many people got the full dose. The trial sponsor, Biogen, did an interim analysis one year before the end and they were concerned about results and stopped the trial early — with only half of the participants completing it. They later analyzed all of the available data and found that one trial was positive and the other was not. Biogen then submitted the drug to the FDA for approval. The FDA granted accelerated approval giving patients with this devastating disease access to a drug that lowers amyloid with the requirement for an additional study to confirm the clinical benefit.
Q: There are physicians and scientists who disagree with the FDA’s decision to approve the drug at this stage and based on the available evidence. What is your response to the concerns they’ve raised?
I understand the concerns about the data, but I believe that the totality of the evidence—clear amyloid lowering and two out of three trials with clinical benefit—as well as the severity of the condition favor accelerated approval. I support the FDA’s requirement for the additional study to confirm the positive results; I think that’s the right thing to do. I think they’re trying to find a balance between making this treatment available for a devastating illness without having to wait another five years but also requiring more data and careful monitoring of patients. This approval, in my opinion, will accelerate Alzheimer’s research. For example, we know the drug isn’t for every patient, so we have to figure out why. Also, candidates will be determined through screening, so that means we need to find better, more efficient and accessible ways to screen patients. I see this as an advance that requires researchers to push ahead.
Q: What patients are the best candidates for treatment with aducanumab?
The best candidates for this drug are those in the early stages of Alzheimer’s, who show signs of mild cognitive impairment and mild dementia. That means there is objective memory loss but the person is still functioning pretty independently, although they may need a bit of assistance. They also need to show amyloid buildup in the brain: only those people that have amyloid plaques will be eligible to receive the medicine. It’s very important to note that this drug is not intended for those with advanced Alzheimer’s or dementia, who have advanced memory loss or moderate or severe cognitive or physical impairment — it hasn’t been tested on patients in the later stages of Alzheimer’s.
Q: What has been your experience in treating patients with the drug?
The memory programs at Butler Hospital and Rhode Island Hospital together probably contributed the largest number of patients to these trials. I’ve personally been treating over 65 patients with aducanumab, and I am so grateful to them for volunteering to be a part of this research. These people really took a risk by stepping into the unknown. Some have been receiving monthly infusions of this experimental medicine for over five years. They tell us they wanted to do this to hopefully protect their children and grandchildren and other people’s children and grandchildren from Alzheimer’s. It’s incredibly inspiring, and I’m thrilled that this approval means they get to witness some of the results of their participation. The majority of the patients I’ve treated have done better than expected. It doesn’t work for everyone, but for some people, it has seemed to slow their decline and they’ve had a better quality of life for a longer time, which is really great.
Q: What are the potential side effects?
This drug is generally very well-tolerated. The main concern is something known as “amyloid-related imaging abnormalities" or ARIA, which can be seen on MRI scans as fluid shifts and small areas of microhemorrhage in the brain. What is happening is that as the drug breaks up amyloid plaques, the fragments move into the bloodstream. Also, some plaque is removed from the walls of the blood vessels in the brain, and can lead to some leakiness of fluid. If this occurs at all, it usually happens early in the treatment and without symptoms. The process is typically reversible and we monitor with MRI until it resolves. This side effect is related to dose, so we have learned to build up on the dose slowly. A higher dose, 10 milligrams per kilogram, has been shown to be the most effective, which is why we need to start lower and build up slowly in order to avoid side effects. People who are carriers of the APOE4 gene for Alzheimer’s also tend to have a higher risk of developing this side effect.
Q: Because the drug is intended only for those with amyloid buildup, what are the next steps in terms of Alzheimer’s screening research?
To treat people with this drug, we need to first screen them for amyloid. And right now the only tools we have to do that are PET scans, which are expensive, and spinal taps, which are invasive. What we need is a blood test that can give us the same information about plaques. That is going to be a key focus of the new Center for Alzheimer’s Disease Research at Brown. We’re building a new fluid biomarker laboratory, which will focus on Alzheimer’s but will also research other neurologic and psychiatric conditions as well. We already have some promising blood tests in the works, and we want to get them ready for clinical use soon as possible. The goal is to be able to do a blood test to see what’s going on in the brain and hopefully integrate that into clinical care to improve access and bring down costs.
Q: What are some other ways this drug affects Alzheimer’s research?
We don’t know for sure, but we’re wondering if perhaps this drug can help people who are at risk of developing memory loss — if we remove the plaques before they show decline, will that delay or prevent memory loss altogether? That’s something we’ll be looking into over the next five years through prevention trials — and we’ll be looking for volunteers. One of the reasons I’m so positive about this approval isn’t just because of this one drug, it’s because of the process that it opens up. We now have a new treatment that lowers amyloid, which is a great start, but hopefully we can combine it with other treatments to have an even bigger impact on the disease. Maybe we can pair it with something that lowers inflammation, or that affects some other component of the disease. That’s the type of discovery research that we plan to carry out at the Center for Alzheimer’s Disease Research, and we’re now in a really great position to move forward.