PROVIDENCE, R.I. [Brown University] — In a toxicology lab at Rhode Island Hospital in Providence, a team of Brown University researchers has been testing samples labeled “biohazard” to discover the precise nature of their toxicity. The bags contain drug residue from discarded drug paraphernalia collected from harm reduction organizations in local communities.
Once samples are tested, findings are disseminated through print flyers, social media posts and emails from the Rhode Island Department of Health. Results are also made available on PreventOverdoseRI.org, the state's overdose dashboard developed through a partnership with the Brown School of Public Health. Sample donors are contacted and provided with information regarding the contents of the residue they submitted for testing. The results can be a surprise — to the sample testers and sample donors alike.
This type of analysis is the cornerstone of TestRI, a new two-year project and study led by Brown researchers and funded by the Foundation for Opioid Response Efforts. There’s an urgent, growing need to test illicit drugs for the presence of additional drugs, according to the research team. Rhode Island, like many parts of the country, is facing an overdose crisis, due largely to the presence of synthetic opioids like fentanyl in the drug supply. Fentanyl can cause overdose even in minuscule amounts, particularly for those who have never encountered it before. If a person doesn’t realize that fentanyl is present in a supply of cocaine or methamphetamines, they have a higher risk of accidentally overdosing.
Other surprise substances can be just as dangerous: one recent TestRI alert warned about the presence of xylazine, used as an animal tranquilizer, in tested samples and advised that not even an emergency treatment of overdose-reversing naloxone may be enough to save a life.
“The drug supply across the U.S. is continuing to change rapidly, and it has left a lot of unknowns,” said Alexandra Collins, an assistant professor of epidemiology at Brown’s School of Public Health. And those unknowns are often deadly. “While there are regional differences, supply contents remain very complex and comprised of a range of synthetic and novel psychoactive substances that can really increase overdose risk.”
TestRI is one of many innovative opioid-focused projects led by scientists, researchers and physicians at Brown University's School of Public Health and Warren Alpert Medical School. From studies on ways to prevent overdoses to evaluating intervention programs and fentanyl test strips to training future physicians to prescribe medications that can help to treat opioid use disorder, Brown faculty, students and staff have spearheaded efforts that make an important difference in the community by taking on the national opioid crisis.
Revealing a drug sample’s true identity
TestRI's work to collect samples is often conducted by Claire Macon, a Brown research assistant. Macon travels around the state in a pickup truck collecting samples at harm reduction organizations and meeting with people who use drugs. The process involves a fair amount of coordination, mileage and gasoline: A sample in Newport might be ready at the same time as a sample in Providence, and both will need to be dropped off at the lab as soon as possible.
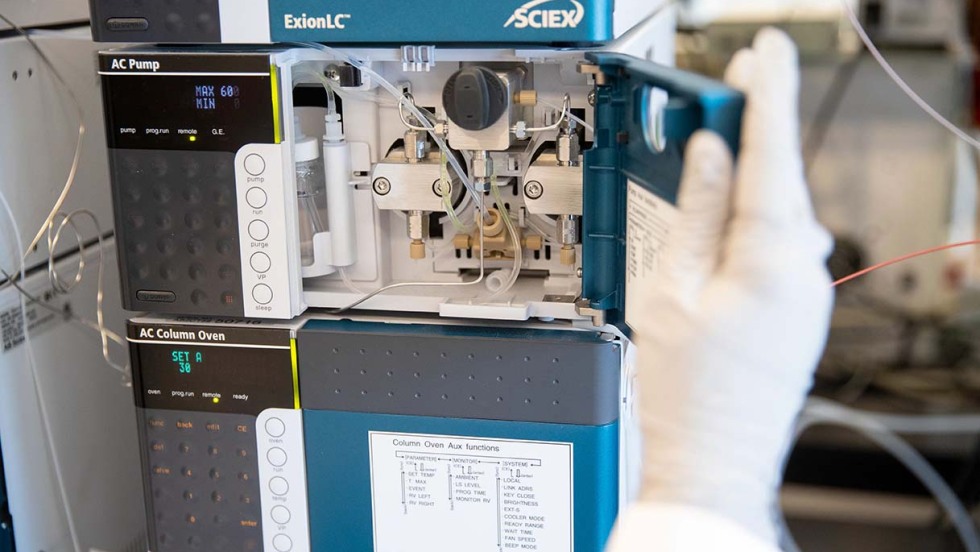
In the lab at Rhode Island Hospital, Adina Badea, director of toxicology at the Lifespan Academic Medical Center, tests the samples using a machine called a liquid chromatography quadrupole time of flight mass spectrometer — its nickname, LC-QTOF-MS, isn’t much shorter — which uses various techniques to determine what chemical compounds are included in a particular sample.
The lab instruments are incredibly sensitive, and detecting the presence of irrelevant substances may invalidate test results, said Badea, who is also an assistant professor of pathology and laboratory medicine at Brown. She changes her gloves frequently to avoid cross contamination.
As part of a demonstration on a July afternoon, Badea pointed to a sample labelled “crack cocaine” and explained that it must be diluted prior to analysis. The mass spectrometer would then run a number of tests on the sample and compare it to a library of pure compounds housed in the lab that serve as analytical standards — like comparing fingerprints, she said. Identifying which specific compounds are in a sample takes about 12 to 14 minutes, and the instrument software produces the results in a matter of seconds.
Then the testers weigh in.