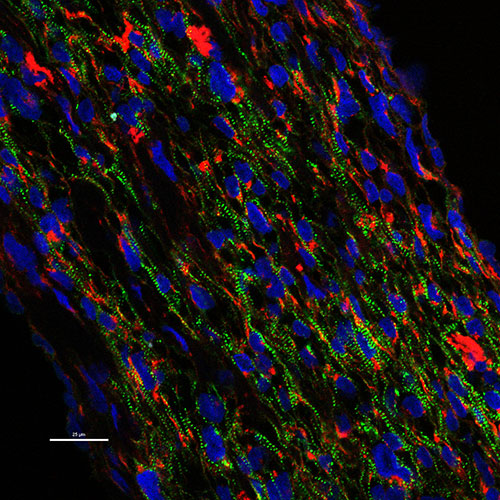
Brown University and LIfespan researchers designed a new way, using a tissue engineering mold, to align human non-embryonic stem cells to derive heart muscle cells to strengthen a rat's heart after a heart attack. The engineered muscle cell bands appear green. The team is led by Kareen Coulombe, assistant professor of engineering, and researchers at Lifespan's Cardiovascular Research Center Ulrike Mende, professor of medicine and Bum-Rak Choi, associate professor of medicine (research). Courtesy Kareen Coulombe
PROVIDENCE, R.I. [Brown University] — Rhode Island’s scientists can deliver the benefits of discoveries more quickly to health care providers and those clinicians can pose more pertinent questions to scientists when they work together closely with broad, deep and cohesive services and support from their academic medical institutions. That’s the vision the Rhode Island Center for Clinical Translational Science (RI-CCTS) will implement with a new $19.5 million, five-year grant from the National Institute of General Medical Sciences.
The grant will allow RI-CCTS to create the educational and technical infrastructure needed to spur Rhode Island researchers to design, conduct and analyze more medical studies, including treatment trials, that build on basic research. The center — based at Brown University in full partnership with the University of Rhode Island and the Care New England, Lifespan and Veterans Affairs hospitals — will also expand the access that medical and public health researchers have to population health data by working with the Rhode Island Quality Institute.
“This $19.5 million grant promises to accelerate the pace at which biomedical discovery can provide medical applications that improve the lives of people in Rhode Island and around the world,” said Brown University President Christina Paxson. “Brown looks forward to working with our academic and medical partners in RI-CCTS to realize the fullest potential of our research, scholarship and service in the community.”
In biomedicine, “translational” means moving an idea along the continuum of basic science, medicine and patient health. When a biologist discovers how one protein interacts with another to cause disease and a biochemist synthesizes a compound to block it, those advances still need to be translated into a safe and effective drug therapy to help patients with the disease. But similarly, if an epidemiologist analyzing statewide health records notices that many people who have one disease also seem to have another health problem, the question of how those might be related can be translated back to scientists who can study the molecular biology at play.
Dr. Jack A. Elias, dean of medicine and biologic sciences at Brown University, said that RI-CCTS will therefore impact health in Rhode Island in many ways.
“Through RI-CCTS we will be better positioned to bring discoveries from the lab to the clinic, we’ll have new tools to analyze and improve patient care, and we’ll endow young scientists and clinicians with the skills to ask the most pertinent questions and to find the answers,” said Elias, the Frank L. Day Professor of Biology and Medicine.
U.S. Sen. Jack Reed, a senior member of the Appropriations Committee who strongly supported RI-CCTS’s competitive grant application, predicted the grant will bring improved health care to patients more quickly.
“This is an exciting award for Brown University and their partners and great news for the state," Reed said. "It will help researchers here in Rhode Island advance scientific breakthroughs in patient care and further enhance economic development by bringing new healthcare innovations to market. These federal funds should provide a real shot in the arm for clinical research and accelerate the process of moving effective discoveries out of the lab and into the community where patients can benefit."
Supporting translational research

Image courtesy Women & Infants Hospital
To achieve those aims, RI-CTTS will create a robust foundation of services and supports and fund dozens of pilot projects and training grants to catalyze new clinical research, said Dr. James Padbury, principal investigator and program director of the new center.
“This is an infrastructure grant,” said Padbury, the William and Mary Oh - William and Elsa Zopfi Professor of Pediatrics for Perinatal Research at Brown’s Alpert Medical School and pediatrician-in-chief at Care New England’s Women & Infants Hospital. “We aren’t being awarded resources to target a specific disease but to build the infrastructure to target a wide range of opportunities.
“Nonetheless, with these resources we will be able to support the kinds of advances that have already been taking place in our own research community — for example, new therapies for asthma and muscular dystrophy; technology for cardiac regenerative medicine; methods for pain management;, national trials on hormone therapy for menopause; the development of vaccines for malaria; the measurement of the effect of home-delivered meals on loneliness in the elderly; and the identification of the link between the mechanisms underlying preeclampsia and Alzheimer’s disease.”

Image courtesy Ed Hawrot
The funding comes from the Institutional Development Award program at the National Institutes of Health, which has supported many local Center of Biomedical Research Excellence (COBRE) grants dedicated to conducting research in areas ranging from behavioral neuroscience to perinatal medicine, cancer and skeletal health. As those centers around the state have emerged over the last decade, local professors and physicians also began to lay the groundwork to earn a grant that would amplify the ability to pursue clinical research.
“There has been a group of faculty across our various institutions who have worked together on this for quite a while,” said RI-CTTS program coordinator Ed Hawrot, Brown’s Alva O. Way University Professor of Medical Science and associate dean of biology. “This has been a great collaboration.”
The structure of RI-CCTS will be built upon seven cores and programs and will create at least 10 jobs, said Helen Leffers, administrative director of the new center: For example, the administrative core will hire four new staff members for functions including communications and finance. As researchers earn funding for pilot projects, they may create additional jobs for the 1-2 year duration of their projects.
- Administrative Core: Led by Padbury, Hawrot and Leffers, the center’s administrative core will be housed at 233 Richmond St. and will manage, coordinate and supervise RI-CTTS operations.
- Pilot Projects Program: Led by medical professors and Providence VA Medical Center physicians Dr. Sharon Rounds and Dr. Michelle Lally, the core will provide 20 seed grants to multidisciplinary teams of junior researchers and mentors to do new clinical research. At least one project each year will be a clinical trial.
- Biomedical Informatics Core: Led by Brown medical professors Neil Sarkar and Elizabeth Chen, this core will provide expertise, training and technological resources to allow for “big data” analyses of medical and genomic data. Sarkar said the grant will accelerate the ability of the Brown Center for Biomedical Informatics to establish a multi-institutional framework for using electronic health data from Lifespan, Care New England and RIQI to enable novel biomedical research opportunities and to support enhanced patient care. This would be among the first such statewide integrations of biomedical, clinical and health data spanning research laboratory, healthcare system and state government sources in the U.S., Sarkar said.
- Clinical Research Design, Epidemiology and Biostatistics Core: Led by Brown School of Public Health biostatistics professor Chris Schmid and Lifespan Biostatistics Core Director Jason Machan, this core will create a central “storefront” of statewide resources and services, mentoring and training, and tools and methods development for conducting well-designed clinical research.
- Professional Development Core: Led by Ira Wilson, chair of health services, policy and practices in the Brown University School of Public Health, the core will provide Mentored Research Awards to three scholars each year. It will also create training programs and develop a statewide mentoring network for clinical and translational research.
- Clinical Research Resources and Facilities: Led by Rhode Island Hospital Clinical Research Center Medical Director Dr. Bharat Ramratnam, this core will unify the many successful clinical research enterprises among partner institutions (encompassing 700 researchers) into a general Clinical Research Center to share best project management and other practices and to gain cost efficiency in setting up and conducting clinical research.
- Tracking and Evaluation Core: Led by University of Rhode Island pharmacy professor Cynthia Willey and Hasbro Children’s Hospital pediatric immunologist Dr. Anthony Hayward, this core will ensure that the center’s work is aligned with program goals and community needs and uses resources wisely. The core will also track the center’s output and monitor progress and practices to achieve continuous process improvement in the center’s work.
“After years of preparation and team building across the state, it is now time for implementation of a highly coordinated statewide effort to advance biomedical research in the full spectrum of translational areas that are most likely to have a positive impact on improving health and diminishing health disparities in Rhode Island,” Hawrot said.