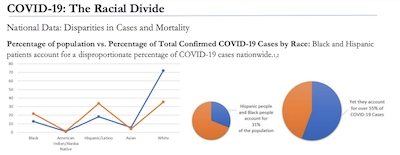
 In the early stages of the COVID-19 pandemic, information about how the virus was spreading and weaning its way through the country quickly revealed that Black, Hispanic, and Native communities bore a strikingly disproportionate burden of the disease. Data emerged to demonstrate that these racial minorities contract and suffer from complications of COVID-19 at higher rates than their white counterparts.(1,5) Many are concerned about the future implications of the virus, and yet we must also confront the long history of discrimination within and outside of the health system that set the stage for these disparities. The racial divide seen within the COVID-19 pandemic is one of many disturbing health inequalities that reveal historical inequities in housing, employment, access to care, and quality of care. These important inequities are summarized below:
In the early stages of the COVID-19 pandemic, information about how the virus was spreading and weaning its way through the country quickly revealed that Black, Hispanic, and Native communities bore a strikingly disproportionate burden of the disease. Data emerged to demonstrate that these racial minorities contract and suffer from complications of COVID-19 at higher rates than their white counterparts.(1,5) Many are concerned about the future implications of the virus, and yet we must also confront the long history of discrimination within and outside of the health system that set the stage for these disparities. The racial divide seen within the COVID-19 pandemic is one of many disturbing health inequalities that reveal historical inequities in housing, employment, access to care, and quality of care. These important inequities are summarized below:
Housing: One of the most comprehensive measures for preventing the spread of COVID-19 is social distancing. However, the ability to effectively socially distance is impacted by access to housing and the condition of living spaces. Consider that nearly 40% of the homeless population in the United States is Black,(6) and both Black and Hispanic people are more likely to inhabit substandard homes and experience housing instability.(7) These disparities are not accidental either, decades of federally endorsed redlining ensured that racial minorities, particularly individuals who identify as Black, were excluded from homeownership and segregated into communities with relatively high costs of living and poorly maintained neighborhoods.(8) Residential segregation has been linked to a variety of adverse health outcomes (including asthma, diabetes, and hypertension) many of which exacerbate the severity of infection with COVID-19.(9)
Employment: While many workplaces have gone remote or temporarily closed offices to stem the transmission of the virus, other businesses and organizations considered “essential” continue to operate. Employees in the service industry, agricultural workforce, and healthcare are all but obliged to continue working in order to keep society afloat, despite the risks to their health. A disparate proportion of service workers are Hispanic and Black, 53% of agricultural workers are Hispanic, and 30% of nurses are Black, creating a sharp racial divide between those who are privileged to work from home and those whose jobs are less accommodating.(10) In addition, Black and Hispanic workers have less access to paid sick leave, effectively limiting their opportunities to reduce transmission of the virus without compromising their economic security.(11)
Access to Care: When Black and Hispanic populations contract the virus there are various barriers that stymie their ability to seek the care they need. They tend to be segregated into communities farther from the medical facilities necessary to test and treat them for COVID-19.(13) In addition, Black and Hispanic adults are more likely to be uninsured than whites and thus less able to afford expensive medical procedures for the myriad complications they are at higher risk of experiencing due to underlying conditions.(12) Access to health insurance has been compromised across the country as millions lose employer-sponsored insurance plans amidst pandemic lay-offs, and rates of unemployment are rising particularly fast among Black workers.(14)
Quality of Care: Where you live impacts your access to care as well as the quality of the care you receive. Because racial minorities and white communities are segregated into different neighborhoods, they have access to different health facilities. Hospitals and clinics in Black communities tend to be under-resourced and populated with less competent providers, less diagnostic and technological supplies, and higher incidences of negligent adverse events.(9) These disparities produce poorer healthcare outcomes and propagate higher mortality rates seen among Black patients.
Inequities of these kind are pervasive and beget other health disparities among racial minorities. A comprehensive response to COVID-19 will require that we address the root causes of all these health disparities and grapple with the history of discrimination and injustice which continually threatens the lives of Black and Hispanic populations.
References
1. Centers for Disease Control and Prevention. (2020, June 05). Cases in the U.S. Retrieved June 11, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
2. US Census Bureau. (2010). Overview of Race and Hispanic Origin. [Census brief]. Retrieved from: https://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf
3. Artiga, S., Garfield, R., & Orgera, K. (2020, April 08). Communities of Color at Higher Risk for Health and Economic Challenges due to COVID-19. Retrieved June 11, 2020, from https://www.kff.org/coronavirus- covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to- covid-19/
4. Gross, C. P., Essien, U. R., Pasha, S., Gross, J. R., Wang, S., & Nunez-Smith, M. (2020). Racial and Ethnic Disparities in Population Level Covid-19 Mortality. doi:10.1101/2020.05.07.20094250
5. RIDOH. (2020, April 28). RI Department of Health COVID-19 Response Data Hub. Retrieved June 11, 2020, from https://ri-department-of-health-covid-19-data-rihealth.hub.arcgis.com/
6. Henry, M., Watt, R., Mahathey, A., Ouellette, J., & Sitler, A. (2020, January). The 2019 Annual Homeless Assessment Report (AHAR) to Congress (Rep.). Retrieved June 10, 2020, from The U.S. Department of Housing and Urban Development website: https://files.hudexchange.info/resources/documents/2019-AHAR-Part- 1.pdf
7. Jacobs, D. E. (2011). Environmental Health Disparities in Housing. American Journal of Public Health, 101(S1). doi:10.2105/ajph.2010.300058
8. Mitchell, B. (2018, December 18). HOLC "redlining" maps: The persistent structure of segregation and economic inequality " NCRC. Retrieved June 11, 2020, from https://ncrc.org/holc/
9. Landrine, H., & Corral, I. (2009). Separate and unequal: residential segregation and black health disparities. Ethnicity & disease, 19(2), 179–184.
10. Centers for Disease Control and Prevention. (2020, June 04). COVID-19 in Racial and Ethnic Minority Groups. Retrieved June 11, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/need-extra- precautions/racial-ethnic-minorities.html
11. Kortrey, J. (2018). Paid Family and Medical Leave: A Racial Justice Issue – and Opportunity (Issue brief). National Partnership for Women & Families.
12. Kaiser Family Foundation. (2019, December 04). Uninsured Rates for the Nonelderly by Race/Ethnicity. Retrieved June 11, 2020, from https://www.kff.org/uninsured/state-indicator/rate-by- raceethnicity/?currentTimeframe=0
13. Tung, E. L., Hampton, D. A., Kolak, M., Rogers, S. O., Yang, J. P., & Peek, M. E. (2019). Race/Ethnicity and Geographic Access to Urban Trauma Care. JAMA Network Open, 2(3). doi:10.1001/jamanetworkopen.2019.0138
14. Gould, E., & Wilson, V. (2020). Black workers face two of the most lethal preexisting conditions for coronavirus—racism and economic inequality (Rep.). Washington, D.C: Economic Policy Institute.
